Abstract
Background. In recent years, the number of Hodgkin Lymphoma (HL) patients submitted to reduced intensity haploidentical allogeneic transplant (RIC haplo SCT) consistently increased. [Sureda et al. Curr Treat Options Oncol 2014] However, with a post alloSCT relapse rate so high as 40-60%, disease control after autoSCT relapse remains a clear unmet medical need. In respect of improving transplant outcome identification of factors influencing outcomes are warranted
Methods.We reviewed outcomes obtained in 44 consecutive HL patients who received RIC haplo SCT between September 2009 and June 2015 at our institution. The donor was haploidentical relative in all cases. All patients had received at least 3 conventional chemotherapy lines before RIC haplo SCT; most of them (72%) were refractory to front-line chemotherapy and all but one had received an autologous SCT. All patients received the same reduced intensity conditiong regime, and GvHD prophilaxis with post-transplant cyclophosphamide (Raiola et al. BBMT 2008). The median age was 31years (range 18-60). Deauville five-points scale were used to interpretate the results of pre-transplant positron-emission tomography (PET) studies, with a threshold of 4 or above considered positive. Survival curve and GvHD incidence were calculated with the method of Kaplan and Meier. Cox regression model was performed to identify pre-transplant factors influencing outcomes.
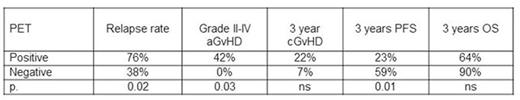
Results. All patients engrafted but 1 who showed autologous recovery. The median day for 500 neutrophils was 15 days (13-23). Three patients died in remission at 8 (cGvHD), 16 (myocarditis) and 51(pneumonia) months from SCT, respectively. Three years non relapse mortality = 8%. Risk of grade II-IV acute GvHD and 3-year chronic GvHD were 22 and 21%, respectively. With a median follow-up for surviving patients of 38 months (range 13-83), 21 relapsed (47%). All relapsed patients were treated with further therapy, mainly immuno-chemotherapy and donor lymphocyte infusion (DLI). The 3-year overall (OS) and progression free survival (PFS) were 77% and 39%, respectively. Pre-transplant PET status was the only factor influencing outcomes of the procedure (OR 5.4; 95% CI 1.7 - 16.6). In the 41 patients with available pre-transplant PET status, 19 were positive and 22 negative. Outcomes accordingly to pre-transplant PET status are shown in the following table.
Conclusions.Pre-transplant PET status is a factor influencing outcomes of relapsed/refractory HL submitted to RIC haplo SCT. Grade II-IV aGvHD was markedly reduced in patients with metabolic remission at time of transplantation.
Angelucci:Novartis oncology, celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal