Abstract
Introduction: Consistent with more direct measures of body fat, body mass index (BMI), defined as a personfs weight in kilograms divided by the square of his height in meters (kg/m2), is strongly correlated with various adverse health outcomes. Recent studies have reported the prognostic benefits of higher BMI at diagnosis in acute myeloid leukemia (AML). However, there are few reports on the prognostic impact of BMI classification and post-remission therapy, including hematopoietic stem cell transplantation (HSCT). Although some studies have reported worse outcomes related to lower BMI at transplant, there are no studies on the prognostic impact of the difference-BMI (d-BMI) between time of transplant and time of AML diagnosis. We hypothesized that lower BMI at transplant and reductions in BMI from diagnosis are associated with worse survival outcomes, including graft-versus-host disease-free survival, relapse-free survival (GRFS), which is currently defined as a novel composite endpoint in the first post-HSCT year.
Patients and Methods: We identified 369 patients from January 2000 to March 2015 newly diagnosed with adult AML who had been administered daunorubicin or idarubicin in combination with cytarabine as induction chemotherapy (IC) at any of the seven Japanese hospitals that collaborate to form the Yokohama Cooperative Study Group for Hematology. Patients with acute promyelocytic leukemia, myeloid sarcoma, and aged 66 years or more were excluded from this study. For adjustment treatment intensification, patients who had over 20% reduction in actual dosage of IC were also excluded. In this study model, 184 patients were eligible for HSCT. According to the classification of obesity by the World Health Organization, underweight patients were characterized by BMI of <18.5 kg/m2, normal weight by BMI of 18.5-25 kg/m2, overweight by BMI of 25-30 kg/m2 and obese by BMI of >30 kg/m2. d-BMI was calculated as BMI at the time of transplant subtracted from BMI at the time of diagnosis, which reflects constructive changes in body structure due to intensive chemotherapy. Based on the ranges of d-BMI, patients were divided into three groups: under −2, between −2 and +2, and over +2. We analyzed overall survival (OS), disease-free survival (DFS), and GRFS in different BMI groups at transplant and in d-BMI groups.
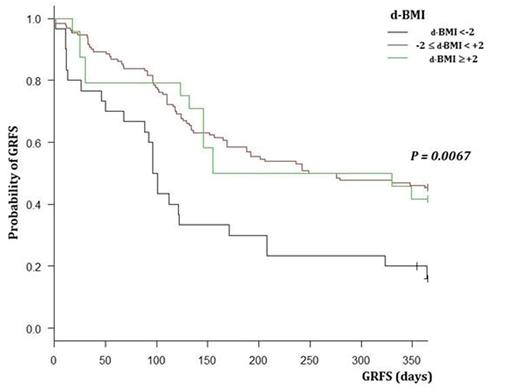
Results: This study included 115 males and 69 females, with median age of 43 years (range, 17-65 years) at diagnosis. In BMI classification at transplant, 29 patients were underweight, 116 were normal weight, 30 were overweight, and nine were obese. At transplant, median BMI was 22.1 kg/m2 (range, 14.8-33.2 kg/m2) and median d-BMI was −0.39 (range, −7.9-+10.0). There were no significant differences in basement characteristics of patients at transplant and in each BMI and d-BMI group. Survival outcomes were observed with a median follow-up period of 1081 days (range, 8-5230 days). At 1 year, OS was 67.9% (95% CI, 60.7-74.2), DFS was 64.1% (95% CI, 56.7-70.6), and GRFS was 40.2% (95% CI, 33.1-47.2). There was no significant association between BMI at transplant and survival outcomes. GRFS at 1 year for the d-BMI groups under −2, between −2 and +2, and over +2 was 16.1% (95% CI, 5.1-31.4), 45.4% (95% CI, 36.4-53.7), and 41.7% (95% CI, 22.2-60.1), respectively (P = 0.0067) (Figure 1). Multivariate analysis showed that a worse GRFS was associated with lower BMI at transplant than that at diagnosis (d-BMI < −2) (HR 2.72, 95% CI, 1.47-5.03, P = 0.015) and the other prognostic factors of performance status (PS) and disease risk.
Conclusions: Our results showed that among 184 AML patients who underwent HSCT for the first time, those with d-BMI < −2 had worse GRFS.
GRFS of patients with newly diagnosed AML according to d-BMI.
GRFS of patients with newly diagnosed AML according to d-BMI.
Fujita:Chugai Pharmaceutical Co.,LTD: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal