Abstract
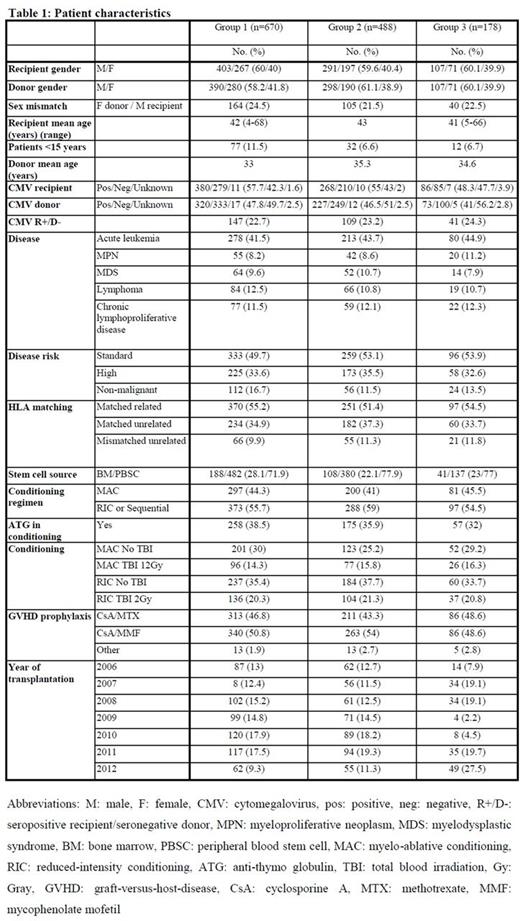
Treatment-related mortality (TRM) after allogeneic hematopoietic stem cell transplantation (HSCT) is a major concern and remains difficult to predict adequately. Several pre-transplant characteristics of patients and disease are associated with TRM. Comorbidity indexes, including pre-transplant assessment of mortality (PAM) and the hematopoietic cell transplantation comorbidity index (HCT-CI), have been developed in an attempt to predict TRM. Biologic markers, such as ferritin, C-reactive protein (CRP) and, more recently, telomere length, also correlate with TRM. However, the cumulative impact of these factors on TRM has not been addressed. Here, we investigated the impact of pre-transplant clinical factors, comorbidity indexes and biologic markers on TRM in 670 consecutive patients from a single center who received a first allogeneic HSCT between January 2006 and June 2012. Clinical factors considered were: year of transplantation, donor and recipient ages, gender and CMV serological status, disease risk (based on the American Society for Blood and Marrow Transplantation Request for Information 2006 risk scoring schema), stem cell source, and HLA matching. Comorbidities were evaluated by PAM and HCT-CI, and coded prospectively for all patients by a single observer. HCT-CI and PAM scores were ranked into previously published categories (0, 1-2, ≥3 for HCT-CI and 9-16, 17-23, 24-30 and 31-44 for PAM; Sorror, Blood 2005; Parimon, Annals Intern. Med. 2006). Ferritin, CRP and biological data for comorbidity indexes were recorded within 2 weeks prior to HSCT. Recipient telomere lengths were determined in peripheral blood leukocytes by qPCR and adjusted for age by the telomere attrition rate observed in donors.Our analysis categorized the population into quartiles and divided patients into 2 groups: shorter telomeres (first quartile) versus longer telomeres (upper 3 quartiles). The entire patient cohort was subsequently divided into 3 groups by data availability: Group 1 (G1), the entire population (n=670) for whom all clinical data were available; G2, 488 patients with clinical and comorbidity index data (pulmonary function tests were not systematically performed during the early study period); and G3, for whom pre-transplant telomere length was available (n=178). Univariate and multivariate methods developed by Fine and Gray for competing risks studies were used to assess prognostic TRM factors, with relapse as a competing event. Table 1 shows patient characteristics. Significant differences between G1 and G2 were found for mean donor and recipient ages, sex mismatch, HLA matching, stem cell source, disease risk, and year of transplantation. Median follow-up was 36 months, overall survival at 5 years for the entire cohort was 60%, and TRM was 18%. In G1, factors significantly associated with higher TRM in multivariate analysis were: recipient age (HR, 1.02, 95%CI [1.0-1.03], p=0.005), CMV seropositive recipient/seronegative donor (R+/D-) (HR, 1.98, 95%CI [1.34-2.92], p=0.001) and mismatched unrelated donor (MMUD) (HR, 2.28, 95%CI [1.38-3.74], p=0.001). In G2, the same factors [recipient age (HR, 1.01, 95%CI [1.00-1.03], p=0.027), CMV R+/D- (HR, 1.91, 95%CI [1.22-2.99], p=0.005), MMUD (HR, 2.55, 95%CI [1.48-4.42], p=0.001)] were associated with higher rates of TRM, whereas PAM showed a trend for higher TRM (HR, 1.41, 95%CI [0.99-1.99], p=0.05). HCT-CI, ferritin, and CRP were not associated with TRM. In G3, only MMUD (HR, 2.82, 95%CI [1.06-7.46], p=0.037) was associated with higher TRM. However, in analysis restricted to patients transplanted from an HLA-matched related or unrelated donor, recipient age (HR, 1.03, 95%CI [1.00-1.06], p=0.027) and telomere length (HR, 2.45, 95%CI [1.07-5.59], p=0.033) were independently associated with higher TRM. This is the first study to investigate the impact of clinical and biological pre-transplant factors and comorbidity indexes on TRM after allogeneic HSCT in a large cohort of patients. Best results were obtained with young patients transplanted from an HLA-matched donor, with CMV other than R+/D-. High comorbidity scores (evaluated by PAM) were marginally associated with higher TRM. In G3 (pre-transplant telomere length available), only HLA-mismatch was significantly associated with higher TRM.
Peffault De Latour:Novartis: Consultancy, Honoraria, Research Funding; Pfizer: Consultancy, Honoraria, Research Funding; Amgen: Research Funding; Alexion: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal