Abstract
Introduction. Anti-thymocyte globulin (ATG) was added to the BuCy conditioning regimen to reduce the risk of rejection in patients undergoing BMT for SCA by the French group. Since then it has been widely used as part of conditioning regimens in SCD patients. However, it remains unknown whether ATG has any effect on survival in these patients. Here we compare outcome of BMT in 17 SCA patients who received Thymoglobulin (rabbit ATG, Genzyme) before transplantation to 33 patients who did not.
Methods. Between July 2004 and November 2015, 50 consecutive patients of 1.7-17.1 years of age with SCA received their first BMT from HLA-identical sibling donors. Of these patients, 17 were prepared for transplantation with oral (n=5) or weight-based iv Bu Cy200 ATG 10 (ATG group) and 33 patients with Fludarabine 150 iv Bu Cy200 (non-ATG group). GVHD prophylaxis consisted of CSA/Methylprednisolone/short MTX. The two groups showed similar patient demographics. Sixty five percent of patients in the ATG group versus 6% in the non ATG group (p=0.00002) were on regular chronic blood transfusion.
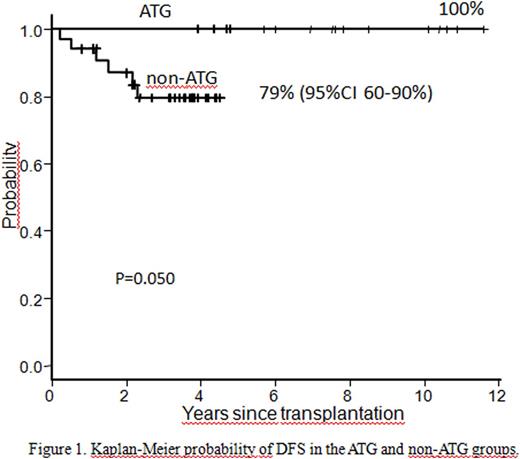
Results. All 50 patients had sustained engraftment. Platelet and neutrophil engraftment kinetics were similar between groups. There was no difference in the incidence of acute or chronic GVHD between the 2 groups. The incidence of grade 2-4 aGVHD in the ATG and non-ATG groups were 35% (95% CI 8-55%) and 33% (95%CI 15-48%), respectively. The incidence of grade 3-4 aGVHD was 0% in the ATG, and 20% (95%CI 4-33%) in the non-ATG group (p=0.07). The incidence of moderate or severe chronic GVHD were 11% (95% CI 0-25%) in the ATG and 22% (95%CI 5-34%) the non-ATG group (p=0.4). At the time of survival analysis, all 17 patients in the ATG group and 27 patients in the non-ATG group were alive, with median follow-up durations of 7.5 years (range, 3.9-12 years) and 3.6 years (range, 0.8-4.5 years), respectively. For all patients the probability of disease-free survival (DFS) was 87% (95% CI 73-94%). DFS was superior in the ATG group (100%) compared with the non-ATG group [79% (95%CI 60-90%)] (P=0.050) (Figure 1). In the non-ATG group 6 patients have died from severe acute or chronic GVHD-related complications.
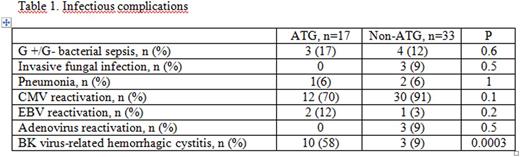
There was no significant difference in the rate of infectious complications between groups, except for a high incidence of BK virus-related hemorrhagic cystitis in the ATG group (Table 1). The incidence of CMV reactivation was high in both groups but none of the patients developed CMV disease. Two patients in the ATG and one in the non-ATG group showed EBV reactivation with low viral load and none of them developed lymphoproliferative disorder. Neurotoxicity related to cyclosporine was similar in both groups (17% vs 15%). At present all patients in the ATG group and 2 patients in the non-ATG group are off immunosuppressive medication.
Conclusions. From this single center study, we report excellent DFS in SCA patients who received ATG as part of the conditioning regimen. This is the first reported study comparing outcomes after ATG-based vs non-ATG-based conditioning regimen for SCA. There was a trend, not significant (p=0.07), for less grade 3-4 aGVHD with ATG in the conditioning regimen. This study showed that the addition of fludarabine to the standard BuCy regimen was well tolerated, and successfully prevented graft rejection in SCA patients. Further study, using low dose ATG in the FluBuCy regimen to increase DFS is currently in progress.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal