Abstract
Abstract
Background: Hematopoietic progenitor cell (HPC) transplantation can cure sickle cell disease (SCD). Anonmyeloablative conditioning regimen has lower morbidity and mortality, and typically results in donor-derived erythrocytes and stable mixedchimerism of recipient- and donor-derived leukocytes. There is a risk ofimmunohematologic complications due to red cell antibodies induced by transfusions during theperi-transplantation period or exposure to donor antigens from the HPC graft. We described the incidence ofimmunohematologic complications in a cohort of patients with SCD undergoing HPC transplantation.
Study design and methods: All patients with SCD (42 with HLA-matched and 19 withhaploidentical donors) enrolled in 3 clinical trials before March 31, 2015, were retrospectively evaluated for the formation of new red cell antibodies after transplantation or any red cell incompatibility between donor and recipient.
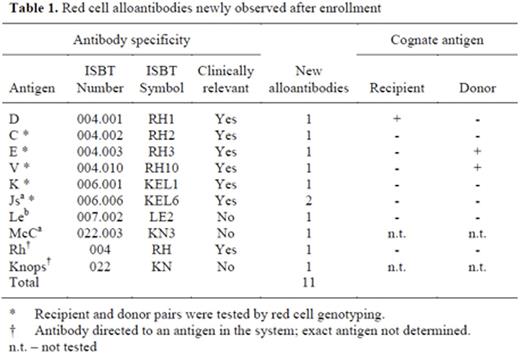
Results: Of the 61 patients, 9 experienced immunohematologic complications. Before HPC transplantation, 3 patients had antibodies that were incompatible with their donors. After HPC transplantation, new antibodies were observed in 6 patients (11 allo-, 2 auto-), 3 of whom developed antibodies that were incompatible with donor or recipient red cells, while 3 developed antibodies that were compatible. The occurrence of new alloantibodies was not significantly associated with allo- or autoantibodies at enrollment, number of pre-enrollment transfusions, recipient sex, or ABO blood group. On average, the 3 patients with antibodies at enrollment that were incompatible with donor red cells received more red cell transfusions and depended on transfusion for longer time periods than comparison groups (51 vs. 13 units, p=0.015; 419 vs. 38 days, p=0.009). Among the 9 patients withimmunohematologic complications, the clinical course was highly variable: some had no significant effects attributable to the antibodies, while others experienced prolongedreticulocytopenia, severe anemia, or became almostuntransfusable. In the 47 patients who maintained their grafts long-term,immunohematologic complications did not negatively impact hemoglobin concentration or hemoglobin S expression after transfusion independence. There was no significant correlation betweenimmunohematologic complications and graft failure, rejection or death.
Conclusions:Immunohematologic complications occurred in 15% of patients with SCD undergoingnonmyeloablative HPC transplantation. Clinical effects ranged from seemingly insignificant to potentially fatal. The formation of new antibodies was not predictable. In individuals with SCD, careful evaluation of donor and recipient phenotypes using red cell genotyping aids in preventing and managingimmunohematologic complications.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal