Abstract
Introduction: Umbilical cord blood (UCB) extends the curative potential of stem cell transplantation to adult patients without a suitable donor. The most commonly used myeloablative preparative regimen results in an unacceptably high 6-month treatment related mortality rate of approximately 32% (Barker J et al. Br J Haematol. 2015). In an attempt to reduce treatment related mortality, we piloted a modified myeloablative regimen with total body irradiation (TBI), fludarabine, and thiotepa. We report clinical outcomes from a cohort of patients who received single or double UCBT after conditioning with this regimen.
Methods: Thirty-one consecutive adult patients ≥ 18 years old with hematologic malignancies who underwent single or double umbilical cord blood transplantation at Duke University from 2010 to 2015 were included in this study. The conditioning regimen consisted of thiotepa 5 mg/kg/day i.v. x 2 days (days -11 to -10), TBI 150 cGy twice a day for total nine fractions (1350 cGy days -9 to -5), and fludarabine 40 mg/m2/day i.v. x 4 days (days -5 to -2). Cord blood units were matched to the recipient at 4 or more HLA loci (intermediate-resolution for A and B, high-resolution for DRB1). Graft versus host disease (GVHD) prophylaxis was with tacrolimus (target level 10-15 ng/ml) and mycophenolate mofetil 1000 mg TID. Antimicrobial prophylaxis and supportive care measures including GCSF administration until ANC > 1000 were conducted per institutional protocol. Probabilities of neutrophil and platelet recovery, acute and chronic GVHD, and treatment-related mortality were estimated by the cumulative incidence method. Relapse-free and overall survival rates were estimated by the Kaplan-Meier method.
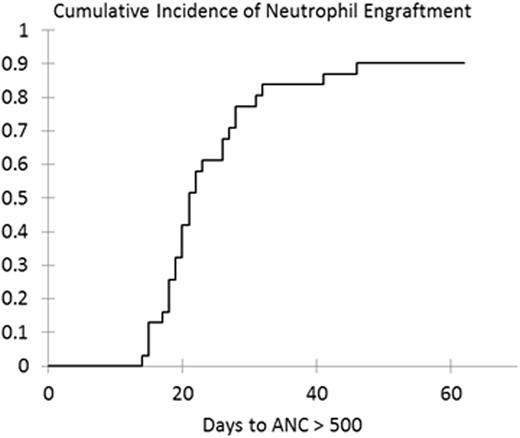
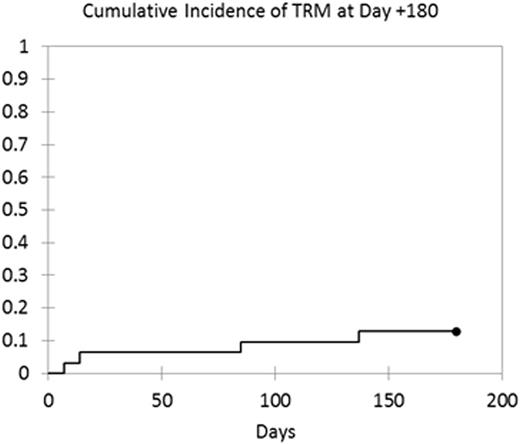
Results: Thirty-one patients (median age 46 years; range, 19-65) with hematologic malignancies were evaluated. Twenty-four patients (77%) had acute leukemia or myelodysplastic syndrome, while 7 patients (23%) had non-Hodgkin's lymphoma or multiple myeloma. By the "Disease Risk Index" (Armand P et al. Blood. 2014), 20 patients (65%) had low or intermediate risk disease, while 11 patients (35%) had high or very high risk disease. 30 patients underwent double UCB and 1 patient received single UCB transplantation. The median cryopreserved total nucleated cell dose was 5.4 x 107/kg (range: 3.2-8.4 x 107/kg). The cumulative incidence of neutrophil engraftment was 90% (95% CI, 82%-99%; Figure 1) at a median time of 21 days (95% CI, 19-26). Three patients did not have neutrophil engraftment; two patients had early death at days 7 and 14 prior to engraftment, while one patient had graft failure requiring second transplant. The cumulative incidence of platelet engraftment was 86% (95% CI, 75%-97%) at a median time of 47 days (95% CI, 37-73). Cumulative incidences of grades II-IV and grades III-IV acute GVHD were 48% (95% CI, 34%-69%) and 10% (95% CI, 3%-28%), respectively. The overall incidence of chronic GVHD was 40% (95% CI, 27%-59%), with 17% (95% CI, 8%-37%) of patients experiencing moderate to severe chronic GVHD. Treatment-related mortality at 6 months was 13% (Figure 2), while at 1 year and 3 years was 27% and 33%, respectively. With a median follow-up of 35.5 months (95% CI, 12.7-52.2), disease-free and overall survival at 3 years was 51% (95% CI, 29%-69%) and 57% (95% CI, 36%-73%), respectively.
Conclusion: UCB transplantation with the modified myeloablative conditioning regimen of TBI, fludarabine, and thiotepa results in reliable neutrophil engraftment with reduced early treatment related mortality as compared to standard myeloablative conditioning consisting of TBI, fludarabine, and cyclophosphamide. It provides a promising disease-free and overall survival in an older (median age 46), heterogeneous patient population. This regimen represents a reasonable alternative to standard conditioning with TBI, fludarabine, and cyclophosphamide and warrants further study.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal