Abstract
Background: Although continued improvement in survival in multiple myeloma was observed over the past decade with the introduction of new therapeutic options such as the proteasome inhibitors and immunomodulatory drugs, the prognosis of myeloma patients (pts) with relapsed and refractory and primary refractory to those drugs is significantly worse than that of responders. The predictive significance of various clinicopathologic characteristics and expression status of osteolysis-related proteins in terms of therapeutic response to bortezomib were evaluated in multiple myeloma pts.
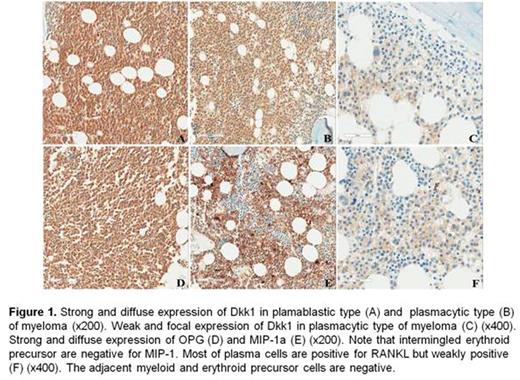
Methods: In 58 pts treated with bortezomib, the clinicopathologic characteristics was retrospectively collected. Pretreatment biopsy samples were analyzed for receptor activator of NF-kB ligand (RANKL), osteoprotegerin (OPG), macrophage inflammatory protein 1 alpha (MIP-1a), and dickkopf-1 (DKK1) expression by immunohistochemistry (Fig 1.).
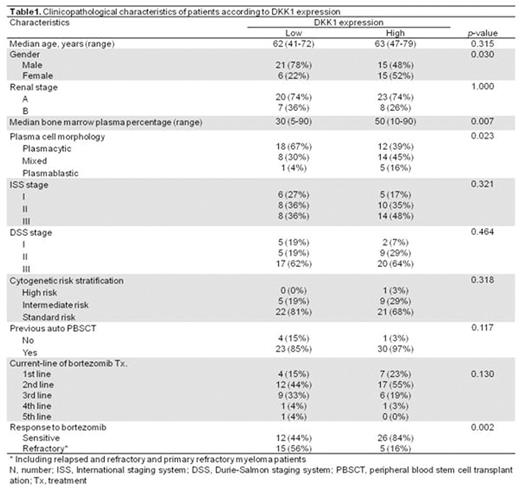
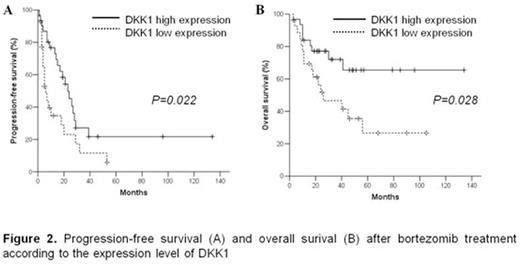
Results: Bortezomib administrated in the fisrt (11 pts), second (29 pts), third (15 pts), fourth (2 pts) and fifth (1 pt) line of chemotherapy. Overall response rate (RR) of bortezomib treatment was 66%. Eight-year overall survival (OS) rate of all pts were 45.3%. Eight-year OS rate of bortezomib non-responders was significantly inferior compared to that of bortezomib responders (24% vs. 62%, p=0.011). The clinicopathologic characteristics including gender, stage, cytogenetic risk stratification by chromosomal aberration and cellularity of bone marrow plasma cell except age and presence of osteolytic lesion were not correlated with response to bortezomib. Median age of bortezomib responders was higher than that of non-responders (65 vs 60, p=0.034). The presence of osteolytic lesion was associated with higher RR of bortezomib treatment (79% vs 46%, p=0.012). High expression of DKK1 was significantly correlated with presence of osteolytic lesion (p=0.003), while expression status of RANKL, OPG and MIP-1a were not associated with presence of osteolytic lesion. In addition, high expression of DKK1 was associated with female gender (p=0.030, Table 1.), increased cellularity of bone marrow plasma cell (p=0.023, Table 1.) and plasmablatic morphology (p=0.007, Table 1.). In multiple myeloma with high DKK1 expression, higher RR was observed (84% vs 44%, p=0.002, Table 1.). In multivariate analysis, high DKK1 expression were independently associated better response to bortezomib (p=0.005). Pts with high DKK1 expression had significantly longer median PFS (23 months versus 6 months, p=0.022, Fig 2A.) and OS (Not reached versus 26 months, p=0.028, Fig 2B.) after bortezomib treatment compared to those with low DKK1 expression. Multivariate analysis revealed that high DKK1 expression was an independent prognostic factor of favorable PFS (p=0.043) and OS (p=0.045).
Conclusion : Despite limitation as retrospective analysis with small sample size, our data indicate that expression status of DKK1 may be a useful predictive and prognostic factor in multiple myeloma pts treated with bortezomib.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal