Abstract
Background: Immunoglobulin light chain (AL) amyloidosis is a fatal complication of B-cell clonal proliferation. Currently, the best biomarker for treatment monitoring is serum free light chain (FLC) assay. Despite its higher sensitivity, it cannot distinguish clonality thus ultralow levels of monoclonal gammopathy can be missed. Urinary exosomes (UExs) are the smallest members of the extracellular vesicle family that are excreted in the urine. They exhibit different characteristics in patients with AL amyloidosis vs multiple myeloma. This study was undertaken to determine if urinary exosomes have different characteristics in patients AL amyloidosis who progress despite being in complete response (CR) vs those who have a renal response.
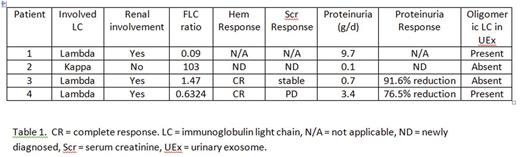
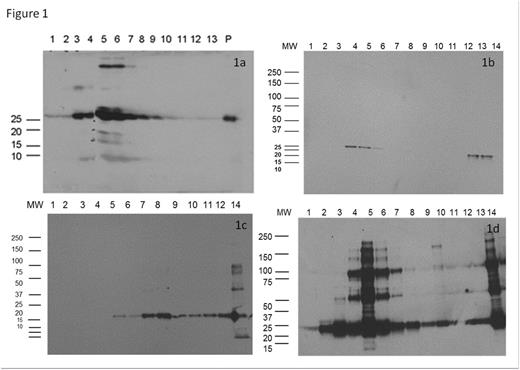
Methods: UEx were extracted from 4 patients at different stages of AL (Table 1). Immunoglobin light chains (LC) were identified in the UEx using western blotting. Intact immunoglobulin light chains were identified in plasma, UEx, and kidney biopsy amyloid deposits using mass spectrometry (MS). cDNAs from bone marrow plasma cells (BMPC) collected at the time of diagnosis from patient 4 were sequened.
Results: Oligomeric LC (250 kd) were identified in the UEx of patient 1 (newly diagnosed, Fig 1a) and 4 (renal progression in CR, Fig 1d) but only monomeric LC (25 kd) were detected in patient 2 (Fig 1b) and 3 (CR and renal response, Fig 1c). MS of the UEx and plasma of patient 4 detected 2 monoclonal λ LC. The mass of one of the LC was consistent with a lambda 6a LC which is also the most common cDNA (IGLV-6-57) found in the BMPC. Amino acid sequences derived from the tryptic digestion of the amyloid deposits matched the predicted sequence of the cDNA. The calculated weight of the peptide produced by the cDNA (23,304 Da ) was within margin of error of the mass of the lambda 6a LC (23,306 Da). The mass of the second LC (23,092 Da) was consistent with a λ4/λ5 LCs. A search of the amino acid and cDNA sequences failed to identify any similarity. The density ratio of the oligomeric LC to monomeric LC in the UEx was 0.47 which was similar to the intensity ratio by MS of the lambda 6a LC (23,306 Da) to the 23,092 Da LC in the blood (0.43).
Discussion: Urinary EXs identified oligomeric LC in a patient with progressive renal disease despite achieving a CR. The mass one of the λ LC matched the predicted peptide product of the cDNA obtained from BMPC. The amino acid sequence predicted by the cDNA matched the trypsin digested sequences from the amyloid deposits. This strongly suggests the oligomeric LC represents the amyloidogenic λ6a LC detected in the blood which was being produced by the BMPC clone which is being deposited as amyloid in the kidney. The origin of the second λ LC is unknown but is likely a new monoclonal gammopathy of undetermined significance that developed after the initial bone marrow biopsy. The blood and urine samples were obtained 3 years after the BMPC. The development of a new monoclonal gammopathy in patients with plasma cell dyscrasia is not uncommon. Unfortunately, bone marrow biopsy collected at the time of the urine and blood sample had insufficient number of plasma cells (CR) for analysis.
Conclusion: UEx can identify amyloidogenic LC even when current standard methods could not. The persistent presence of the amyloidogenic LC helps explain why patients can progress despite being in CR. The presence of a second λ LC which was not part of the amyloid deposit also has clinical implication. It may explain why some patients do well despite having a persistent monoclonal protein. If these results are confirmed, UEx may have a powerful role in the determination of organ and hematologic response in patients with AL amyloidosis.
Dispenzieri:Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; Prothena: Membership on an entity's Board of Directors or advisory committees; Alnylam: Research Funding; GSK: Membership on an entity's Board of Directors or advisory committees; pfizer: Research Funding; Jannsen: Research Funding; Celgene: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal