Abstract
Introduction: Proportion of bone marrow (BM) blasts is a major prognostic factor for outcome in patients with myelodysplastic syndromes (MDS) and is included in the most applied prognostic scoring systems: IPSS and IPSS-R. IPSS-R stratifies patients in five risk categories: very low (VL), low (L), intermediate (I), high (H) and very high (VH). Some concerns exist about the real prognostic significance of intermediate risk group, as these patients showed around 30 months of median overall survival (OS) in different studies. The Spanish Group of myelodysplastic syndromes considers as high-risk patients those with an expected median OS inferior to 30 months. As showed in a recent study of our group, considering BM blasts from nonerythroid cellularity improves the prognostic evaluation of MDS (Arenillas et al, J Clin Oncol 2016) when applying IPSS and WHO classification.
Aims: 1) To assess OS and leukemia-free survival (LFS) prediction by IPSS-R by counting BM blast percentage from nonerythroid cells (NECs). 2) To evaluate whether considering BM blasts from NECs rather than from total nucleated cells (TNCs) improves the prognostic assessment of patients classified into the intermediate risk group. 3) To establish which of these methods present the best prediction capacity for survival and leukemic transformation.
Methods: We retrospectively analyzed 3,924 denovo MDS diagnosed according to WHO 2008 from the MDS spanish registry. Percentage of BM blasts from NECs was calculated as follows: [%BM blasts from TNCs/(100 - %BM erythroblasts) x 100]. Survival curves were constructed by using the Kaplan-Meier (K-M) method and compared using the log-rank test. C-index was implemented to assess the method with the best predictive value for survival and leukemic transformation.
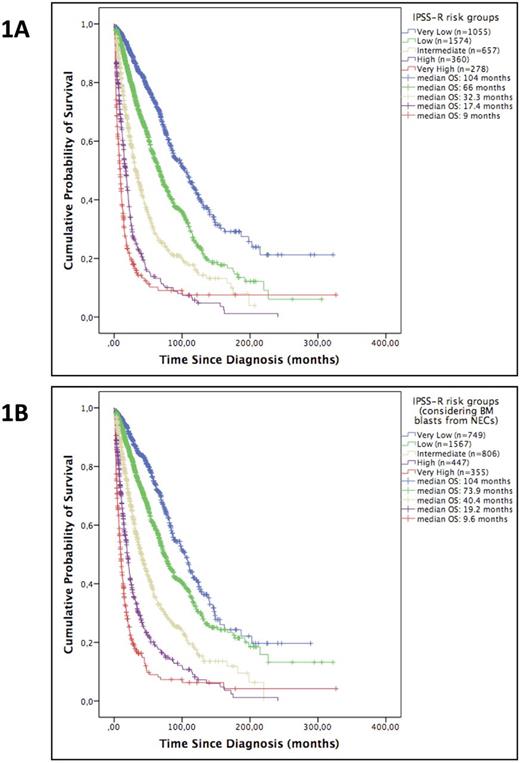
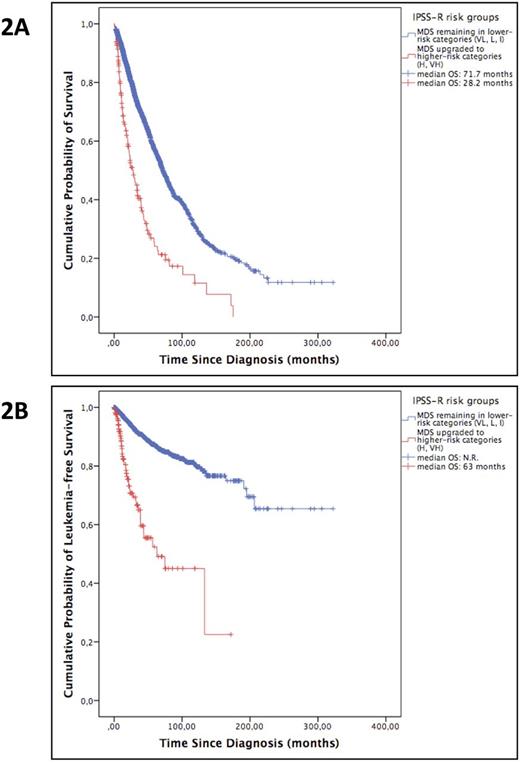
Results: Median age at diagnosis was 75y (16-101y) and 59% were males. Estimated median follow-up, as calculated by reverse K-M method, was 46.5 months (95% CI, 43.9-49) and median OS was 56.97 months. We assessed OS predicted by IPSS-R by considering BM blasts from TNCs and from NECs (recoded IPSS-R) Fig 1A and 1B. As depicted, five groups with significant differences in OS were observed by using both methods. Interestingly, median OS of intermediate risk group patients changed from 32.3 to 40.4 months by considering blasts from NECs instead of TNCs, whereas patients classified in high and very high risk categories showed almost the same survival even though the higher-risk categories were increased in 25.7%. Of 3,285 patients, 164 (5%) classified in the lower-risk IPSS-R categories (VL, L, I) were reclassified into higher-risk categories (H, VH) when BM blasts were enumerated from NECs. OS and LFS of these upgraded patients was significantly shorter to those observed in patients who remained in the initial categories (median OS, 28.2 vs 71.7 months, P<0.001; median LFS, 63 vs N.R. months, P<0.001) Fig 2A and 2B. In the same way, 24% of patients classified into the intermediate IPSS-R risk group were reclassified into higher-risk categories and showed a significantly shorter OS and LFS (median OS, 24 vs 34.3 months, P=0.012; median LFS, 56.8 vs 164.7 months, P=0.005). Thus, by counting BM blasts from NECs we were able to detect a group of patients labeled at present as having lower-risk disease but who presented an outcome much closer to that of higher-risk patients. The worse outcome observed in these reclassified patients was mainly influenced by the difference in the weight of blasts when assessed from NECs, as other prognostic factors that could explain this difference in outcome, as cytogenetics and degree of cytopenias, were adjusted by using the IPSS-R. Finally, C-index was calculated at 2 and 5 years and the recoded IPSS-R showed a slightly higher value for the prediction of survival and leukemic transformation [(survival, recoded IPSS-R vs IPSS-R: 2y, 0.731 vs 0.728; 5y, 0.696 vs 0.695) (leukemic transformation, recoded IPSS-R vs IPSS-R: 2y, 0.731 vs 0.730; 5y, 0.719 vs 0.716)].
Conclusions: calculating the percentage of BM blasts from NECs improves prognostic assessment of MDS in the context of IPSS-R. By using this method, a more comprehensive distribution of patients was observed, as patients now included in the intermediate risk group presented an outcome much closer to that expected in lower-risk patients. This approach could help clinicians in risk-adapted therapeutic decisions by allowing a better definition of this controversial group.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal