Abstract

Background: The International Prognostic Scoring System published in 1997 (IPSS) was revised (R-IPSS) (Greenberg et al, Blood 2012)in order to better define the prognostic impact on overall survival (OS) for patients diagnosed with myelodysplastic syndrome (MDS). Although red blood cell transfusion dependency (RBC-TD) is associated with poor prognosis in this subset of patients, it was not included in the R-IPSS analysis because of the relatively low proportion of patients with this data available. We hypothesize that the use of RBC-TD status may improve R-IPSS prognostic assessment.
Aim: To assess the impact of RBC-TD in addition to R-IPSS in predicting survival outcome for untreated MDS, acute myelogenous leukemia (AML) (blasts 20-30%) and chronic myelomonocytic leukemia (CMML) patients.
Material and Methods: We identified in our database 686 MDS, AML and CMML untreated patients according to the R-IPSS selection criteria. RBC-TD was defined as having received at least one RBC transfusion every 8 weeks over a period of 4 months (Malcovati et al; JCO 2007). Patients were classified into two groups according to RBC-TD at the time of or before the landmark time point and transfusion independency at the landmark time point. Overall survival (OS) was measured in years since diagnosis. Landmark analyses were conducted at 6,12, 24 and 36 months after the diagnosis and patients who experienced the event (i.e. death) before the landmark time point were excluded.
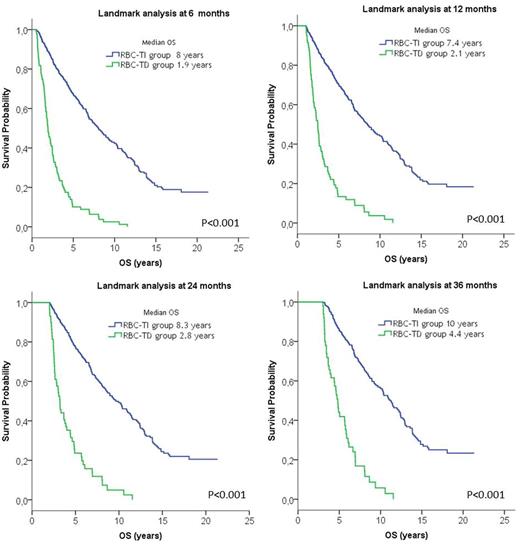
Results: 686 patients were included in the analysis. Median age at diagnosis was 72 years (range 30-101) and 445 (65%) were male. WHO 2008 diagnosis was: 4% CRDU, 10% RARS, 38% RCMD, 17% RAEB-1, 7% RAEB-2, 20% CMML, the remaining 4% were MDS-U and AML (blasts 20-30%). Median OS was lower for male than for female patients (5.3 vs. 7.6 years; p 0.002) and in elderly patients (11.5, 6.6 and 3.4 years in patients <65, 65-80, >80 years respectively (p<0.001). Median OS was 8, 7.6, 3.8, 1.2 and 0.2 years for very low, low, intermediate, high and very high risk group respectively (p<0.001) according to R-IPSS index. Multivariate analysis performed at time of diagnosis and at each landmark analysis included gender, age, R-IPSS and RBC-TD status and indicated that RBC-TD at diagnosis and at or before 6, 12, 24 and 36 months was associated with poor survival, independently of R-IPSS category, age and gender. Median survival for patients who became RBC-TD by 6 months was significantly lower than that of patients who remained RBC-transfusion independent (1.9 vs. 8 years; p<0.001; Fig 1A). Similarly, median OS was significantly lower for patients who became RBC-TD by 12 months (2.1 vs. 7.4 years; p<0.001; Fig 1B), 24 months (2.8 vs. 8.3 years; p<0.001; Fig 1C) and 36 months (4.4 vs. 10 years; p<0.001; Fig 1D).
Conclusions: This single-centre experience confirms the negative impact on survival of TD at the time of diagnosis and at any time during the course of MDS disease. As treatment decisions are based on the initial prognostic risk assessment, the inclusion of transfusion dependency on the risk stratification may provide more precise prognostic information with impact on the therapeutic approach.
Landmark analysis for OS according to RBC-transfusion dependency at 6, 12, 24 and 36 months.
Landmark analysis for OS according to RBC-transfusion dependency at 6, 12, 24 and 36 months.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal