Abstract
Higher Prevalence of Hydroxyurea Use Is Associated with Lower Hospitalization Rate in a Population of Children with Sickle Cell Disease
Cecelia L. Calhoun, MD; Ryan Colvin, MPH; Sherry Lassa-Claxton, MS; Arti Verlekar MS; F. Sessions Cole, MD; Monica L. Hulbert, MD
Background
Individuals with sickle cell disease (SCD) treated with hydroxyurea (HU) in clinical trials have had fewer hospitalizations and vaso-occlusive pain episodes than those on placebo. Since 2014, HU has been recommended for all children with Hemoglobin SS/S-β0 thalassemia, and many SCD centers have increased HU utilization. The effect of expanded HU treatment on hospitalization rate has not been reported in a population of children clinically treated with HU. In a pediatric SCD center cohort, we tested the hypothesis that increasing prevalence of HU treatment was associated with reduced hospitalization rate per patient-year and in total hospitalizations.
Methods
PedsNet, a PCORI-funded clinical research initiative, was queried for all patients with inpatient or outpatient encounters for SCD at St. Louis Children's Hospital (SLCH) from 2010 through 2015. Data from patients with ICD-9 codes indicating any genotype of SCD were included. Patients were considered to be receiving HU when it was prescribed on 2 or more outpatient encounters. Exclusion criteria were lack of SCD diagnosis confirmation, lack of outpatient visits at SLCH, and presence of a significant unrelated medical condition. Patients were censored at their 21st birthday or date of hematopoietic stem cell transplant. Data generated at the adult hospital were excluded. All hospitalizations in the final cohort were included for analysis, regardless of diagnosis code. For comparisons, patients were grouped as having a severe genotype (SS, S-β0 thalassemia, SD) or less-severe genotype (SC, S-β+ thalassemia). Statistical analysis was performed using SAS 9.4. Logistic and Poisson regression were used to compare proportions and rates between groups, respectively. Generalized Estimating Equations were used to account for within patient correlation.
Results
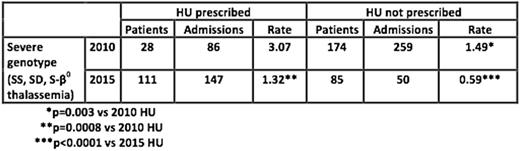
The PedsNet query identified 646 patients. Sixty patients were excluded due to lack of SCD diagnosis, 78 due to lack of outpatient care, and 4 due to severe unrelated disease (3 with congenital disease/malformation, 1 with cancer), leaving 504 who met all inclusion criteria (51.6% male). Hematopoietic stem cell transplant was performed in 23 patients during the study period. Of patients with a severe genotype, 28 (20.1%) received HU in 2010 compared with 111 (65.6%) in 2015 (p<0.0001). Fewer patients in the less-severe genotype group received HU: 5 patients (4.3%) in 2010 and 13 (14.3%) in 2015 (p=0.006). In the severe genotype group, the rate of hospitalizations per patient-year decreased from 1.71 to 1.01 (p<0.0001) and the total number of hospitalizations decreased from 345 to 197. Throughout the study period, HU-treated patients in the severe genotype group had a higher hospitalization rate than HU-untreated patients; both treated and untreated patients had a significantly lower rate in 2015 than 2010 (Table), suggesting that hospitalizations were prevented as children who were more prone to hospitalizations began HU therapy. There was no significant change in hospitalization rate over time in the less-severe genotype group, at 1.13 hospitalizations per patient-year in 2010 and 1.16 in 2015 (p=0.94), with no impact of HU in this group.
Conclusions
In this clinical cohort of children with SCD, increasing prevalence of HU treatment was associated with significantly fewer total hospitalizations and a lower hospitalization rate per patient-year. The constant hospitalization rate in the less-severe genotype group suggests that the reduction is attributable to HU, rather than to other changes in clinical practice affecting patients with all genotypes. Hospitalization rates were higher among HU-treated patients, suggesting that more symptomatic children remain more likely to receive HU despite published recommendations to treat all children with severe genotypes. Families and clinicians may be reluctant to initiate HU for primary prevention of pain and hospitalizations in asymptomatic children. Future work should examine HU effects on specific SCD complications and on costs of care. Family and clinician interventions are needed to promote HU utilization in targeted patient groups.
Hulbert:Pfizer, Inc.: Other: spouse employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal