Abstract
Background: Neurolymphomatosis (NL) is a rare pathological condition of non-Hodgkin lymphoma characterized by infiltration of malignant lymphoma cells into the peripheral nervous system. Patients may develop NL at initial presentation, during disease progression, or as relapse. Diagnosis is often difficult as clinical symptoms of NL are nonspecific and varied. Although nerve biopsy remains the gold standard for diagnosis, it is often unfeasible due to the possible irreversible neurological deficit and its scattered distribution. Prognosis and optimal therapeutic strategy are poorly understood due to its rarity. To clarify the clinical features of NL, we retrospectively analyzed 14 cases of NL with emphasis on diagnosis and treatment. This is a largest series of NL cases as a single institutional report.
Method: We reviewed the clinical records of patients admitted to our hospital from April 1, 2006, to April 30, 2016. Diagnosis of NL required: 1) clinical symptoms and neurological findings related to the peripheral nerves; and 2) histological confirmation of malignant lymphoma cells within these nerves; or 3) CT/MRI demonstration of nerve enhancement and/or enlargement of nerve(s) that were also demonstrated by accumulation of FDG on FDG-PET/CT and/or whole-body diffusion weighted whole-body MRI (DW-WBMRI). We surveyed therapeutic contents and analyzed prognosis.
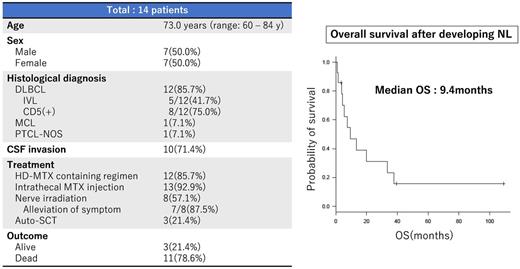
Result: Over the past 10 years, 901 patients with NHL were admitted to our hospital; 14 patients (1.6%) were diagnosed with NL (7 men, 7 women, median age: 73.0 years, range: 60 - 84 years). Twelve patients were histologically diagnosed as DLBCL and 5 of them primarily presented with intravascular lymphoma (IVL). Among the 12 DLBCL patients, 8 were positive for CD5 (75.0%). One patient was originally diagnosed as mantle cell lymphoma (MCL), and another one patient was diagnosed as peripheral T-cell lymphoma not otherwise specified (PTCL-NOS). NL occurred as part of primary disease in 3 patients and as relapse in the remaining 11 patients. All patients were diagnosed with NL by neurological findings and imaging studies (contrast-enhanced MRI, PET/CT, and/or DW-WBMRI). All of the patients with relapsed NL showed neither prominent lymphadenopathy nor abnormal laboratory data except neurological abnormalities. In one patient, NL lesions were evaluated by both PET/CT and DW-WBMRI simultaneously. DW-WBMRI had greater sensitivity for detecting NL lesions than PET/CT. Autopsy also confirmed lymphoma infiltration in one patient. Cerebrospinal fluid cytology was positive in 10 cases (71.4%).
Twelve patients received high-dose methotrexate (HD-MTX) in addition to systemic chemotherapy. Despite initial responses, rapid disease recurrence occurred in all patients. Neurological symptoms responded promptly in 7 of 8 patients receiving involved nerve irradiation (87.5%). Eleven patients (78.6%) died due to progressive NL. Three patients are still alive 109.0, 39.0 and 3.4 months, respectively, from the diagnosis of NL. The median survival after development of NL was 9.4 months (range: 1.0 - 109.0 months). Three patients received autologous stem cell transplantation (auto-SCT), 2 patients survived for more than 7 years free of disease and the other for 1 month just received transplantation, but the remaining one patient relapsed and died 4 months after auto-SCT.
Conclusion: NL is an extremely rare pathological condition (1.6%) and can present in diverse ways, both at initial diagnosis of lymphoma and after treatment. Twelve patients (85.7%) were DLBCL, and 75% of them were CD5-positive. IVL was the most common subtype. Cerebrospinal fluid was positive in 71.4% cases at the time of NL development. Imaging techniques, including contrast-enhanced MRI and PET/CT, are useful and DW-WBMRI may be more sensitive for detecting the relevant neural involvement. Prognosis remains poor once NL has developed despite the use of HD-MTX and rituximab-containing aggressive chemotherapy with or without auto-SCT. Only involved nerve irradiation was effective for temporary relief of neurological symptoms.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal