Abstract
Background: Patients with relapsed/refractory (R/R) mantle cell lymphoma (MCL) have limited treatment options, especially those receiving multiple prior therapies. Patients with MCL are mostly an elderly population with various comorbidities who receive multiple medications that may lead to an increased risk of toxicity from underlying disease, as well as drug interactions. These multiple, concomitant conditions introduce complexity into the evaluation of the risk-benefit ratio of available therapies. In the relapsed setting, there is increasing use of new treatment options, such as lenalidomide, which is an immunomodulatory agent with direct and immune-mediated mechanisms of action. Lenalidomide has shown efficacy and a tolerable safety profile in multiple studies of R/R MCL, including the randomized MCL-002 (SPRINT) study comparing lenalidomide vs. investigator's choice (IC) of monotherapy. The objective of this post hoc subgroup analysis from the MCL-002 study was to examine the effect and safety of lenalidomide in patients who are at risk of bleeding events because of multiple comorbidities or treatments (i.e., polymedication) denoted as LEN-CM compared with those not at risk (LEN), LEN-CM being a population with a limited choice of treatment options.
Methods: The multicenter MCL-002 study randomized patients 2:1 to lenalidomide vs. single-agent IC of monotherapy (rituximab, gemcitabine, fludarabine, chlorambucil, or cytarabine; NCT00875667). Patients had 1-3 relapses or had failed prior therapy, and were ineligible for intensified chemotherapy or stem cell transplantation. Oral lenalidomide was initiated at 25 mg/day on days 1-21 of 28-day cycles until disease progression or as tolerated. Progression-free survival (PFS) was the primary endpoint (per modified 1999 IWG criteria); secondary endpoints included response rates, duration of response (DOR), overall survival (OS), and safety. The current analyses were based on investigator's assessment. Specific patient groups with or without increased bleeding risk due to comorbidities and/or treatment were identified for the subgroup analysis based on pre-existing characteristics at study initiation. Patients in the LEN-CM group included those with hemorrhages (or predispositions to such), concomitant anticoagulant therapy with vitamin K antagonists or nonsteroidal anti-inflammatory drugs, and/or current or preexisting atrial fibrillation requiring anticoagulants.
Results: Of 170 patients originally randomized to lenalidomide treatment, there were 60 (35%) LEN-CM vs. 110 (65%) LEN patients included in this subanalysis. At baseline, patients in both groups generally had a similar baseline patient profile and prior treatment history, although there were some differences between groups: more patients in the LEN-CM group (vs. LEN) were >=65 years of age (78% vs. 62%) and had more high-risk MIPI score at baseline (47% vs. 29%), whereas fewer had positive bone marrow (7% vs. 15%), high tumor burden (37% vs. 54%), or bulky disease (15% vs. 25%).
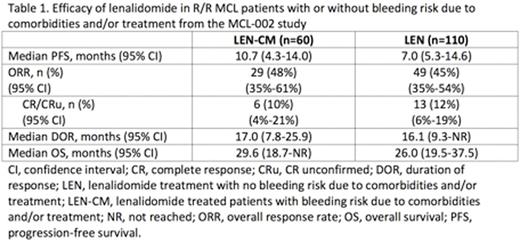
Median PFS by investigator assessment was 10.7 months (95% CI, 4.3-14.0) for LEN-CM and 7.0 months (95% CI, 5.3-14.6) for LEN (Table 1). Overall response rates (ORR) in the LEN-CM vs. LEN patients were 29/60 (48%) and 49/110 (45%) with complete response (CR)/CR unconfirmed (CRu) rates of 6/60 (10%) and 13/110 (12%), respectively. Median DOR and OS were also similar in both groups of lenalidomide-treated patients. The safety profiles were similar for these subgroups, with similar rates of AEs leading to discontinuations and dose reductions/interruptions. Most common any grade treatment-emergent AEs (>=20%) for LEN-CM vs. LEN groups respectively were 48% vs. 52% neutropenia, 33% vs. 38% thrombocytopenia, 32% vs. 27% anemia, 25% vs. 19% fatigue, 23% vs. 22% diarrhea, and 5% vs. 23% pyrexia.
Conclusions: For patients with R/R MCL, there is a high, unmet medical need for effectivetherapy with acceptable toxicity. Overall, the LEN-CM and LEN subgroups showed similar efficacy and safety outcomes. Results from this subgroup analysis of the MCL-002 study show that lenalidomide leads to clinically meaningful PFS and other efficacy outcomes irrespective of the presence or absence of bleeding risk due to comorbidities and/or treatment.
Walewski:Roche: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; GSK: Research Funding; Novartis: Research Funding; Mundipharma: Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Takeda: Honoraria, Membership on an entity's Board of Directors or advisory committees; Janssen Cilag: Honoraria, Membership on an entity's Board of Directors or advisory committees; Teva: Honoraria; Gilead: Honoraria, Membership on an entity's Board of Directors or advisory committees; Sanofi: Honoraria; Servier: Honoraria, Membership on an entity's Board of Directors or advisory committees; Ariad: Membership on an entity's Board of Directors or advisory committees. Belada:Seattle Genetics: Research Funding. Radford:Novartis: Honoraria, Speakers Bureau; Seattle Genetics: Honoraria, Speakers Bureau; GSK: Equity Ownership; Astra-Zeneca: Equity Ownership; Takeda: Consultancy, Honoraria, Research Funding, Speakers Bureau. Jurczak:Morphosys: Consultancy, Research Funding, Speakers Bureau; Acerta: Research Funding; Novartis: Research Funding; Pfizer: Research Funding; Celgene: Research Funding; Gilead: Research Funding; Janssen: Research Funding; Celtron: Research Funding; Bayer: Research Funding; Takeda: Research Funding; Servier: Research Funding; Teva: Research Funding; Roche: Research Funding, Speakers Bureau; Sandoz-Novartis: Speakers Bureau. Morschhauser:Janssen: Honoraria; Celgene: Consultancy, Honoraria; Roche: Consultancy, Honoraria; Gilead Sciences: Consultancy, Honoraria; Servier: Consultancy, Honoraria. Kaplanov:State Budgetary Healthcare Institution "Volgograd Regional Clinical Oncology Dispensary #1: Employment. Thyss:Takeda: Research Funding; Millennium: Research Funding. Kuzmin:Republican Clinical Oncology Dispensary: Employment. Stelitano:Azienda Ospedaliera: Employment. Marks:Pfizer: Honoraria. Trümper:Roche: Research Funding; Mundipharma: Research Funding; Hexal: Membership on an entity's Board of Directors or advisory committees. Biyukov:Celgene: Employment, Equity Ownership. Barnett:Celgene Corporation: Employment, Equity Ownership. Casadebaig Bravo:Celgene: Employment, Equity Ownership. Arcaini:Sandoz: Membership on an entity's Board of Directors or advisory committees; Bayer: Membership on an entity's Board of Directors or advisory committees; Roche: Membership on an entity's Board of Directors or advisory committees; Gilead: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal