Abstract

Introduction:
Somatic mutations are common in MDS and mutation profiling is becoming increasingly standard as part of the initial diagnostic evaluation. The value of serial monitoring of mutation profiles in MDS patients at multiple disease course time points is unknown. We evaluated the impact of serial mutation monitoring in a cohort of MDS patients.
Methods:
MDS patients from participating institutions of the MDS CRC with molecular genetic data by next-generation sequencing available from at least two distinct time points were included in analyses. Mutations present at the first time point were compared to those present at subsequent time points and correlated with age, International Prognostic Scoring System (IPSS) score, and overall survival, measured from diagnosis. Cox proportional hazards model of time from diagnosis to death or loss of follow up with time varying number of mutated genes, gained genes and lost genes adjusted for sex, age at diagnosis, and IPSS category at/near diagnosis was applied.
Results:
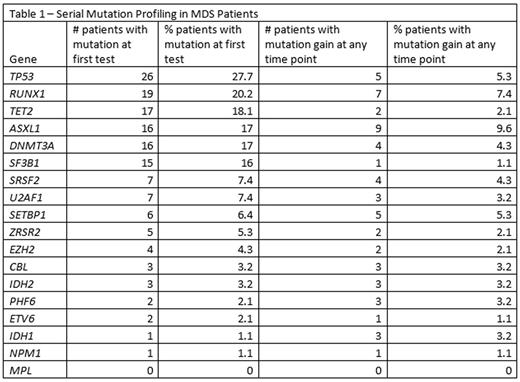
Of 737 MDS patients with molecular genetic data available from 1994 to 2016, 94 had information on the 18 genes presented in Table 1 from at least two distinct time points. Patients had a median of 2 (range 2-9) myeloid mutation panel assessments, with a median interval of 3.3 months (range 0.1-39) between studies. Mutation testing was repeated at the investigator's discretion either at time of suspected disease progression or change of therapy.
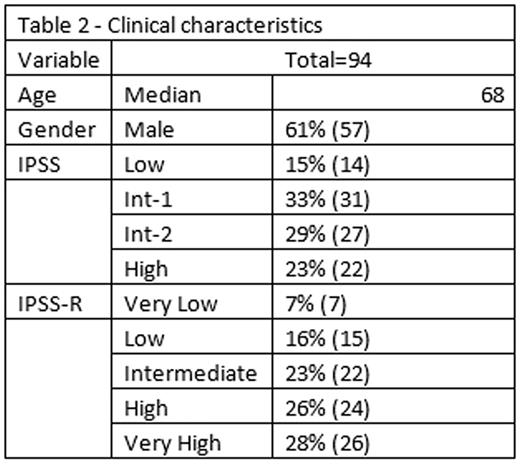
Clinical characteristics of the patients are summarized in Table 2. Almost half (46%) had an initial mutation profile performed within 1 month of diagnosis, 23 patients (24%) within 1-12 months, and 28 patients (30%) more than 12 months after diagnosis. At the time of initial evaluation, patients had a median of 1.5 mutations (range 0-4), with the most common being TP53 (28%), RUNX1 (20%) TET2 (18%), DNMT3A (17%), and ASXL1 (17%). Independent of age or IPSS score at baseline, the number of mutations initially present in a gene set consisting of ASXL1, EZH2, ETV6, RUNX1, TP53 was associated with poor overall survival (HR 2.19, p=0.003, 95% CI, 1.30-3.69). Overall, 32 patients (34%) acquired at least one additional mutation at subsequent testing, including ASXL1 (10%), RUNX1 (7%), TP53 (5%), SETBP1 (5%), and DNMT3A (4%).
The acquisition of additional mutations in any gene in subsequent testing was associated with worse overall survival (HR 1.93, p=0.0002, Cl, 1.36-2.75), irrespective of age, IPSS score, and the number of mutations initially identified among the core group of five prognostically significant mutations. Of note, treatment was similar for patients who were found to have acquired additional mutations compared to those who did not: hypomethylation agents (93% vs 80%, p=0.11), lenalidomide (10% vs 11%, p=0.94), and chemotherapy (38% vs 49%, p=0.33). Patients who acquired at least one additional mutation beyond those identified at diagnosis had a higher rate of acute myeloid leukemia transformation (62% vs 37%, p=0.02). Additional acquired mutations were more likely to be observed in serial testing after AML transformation, compared to patients without AML transformation (36% vs 17%, p=0.01). In this model, acquisition of a mutation in DNMT3A, IDH1, IDH2, SETBP1, or TET2 was associated with poor overall survival (HR 3.88, p=0.006, CI, 1.46-10.3). Gain of mutations in CBL, MPL, NPM1, or PHF6 was also associated with poor survival (HR 8.15, p=0.0008, CI, 2.38-27.86). Loss of mutation in serial testing was observed in 33% of patients was and did not correlate with overall survival (HR 0.66, p=0.25, CI, 0.32-1.36). A small subset of patients who underwent allogeneic stem cell transplantation were found to lose their diagnostic mutation(s) at the time of transplant.
Conclusions:
The acquisition of new mutations in MDS patients undergoing serial monitoring is associated with poor overall survival independent of age, sex, and IPSS, in some part related to the indication for testing. Serial mutation profiling identified a small number of patients who acquired "actionable" mutations for which clinical trials were potentially available, but did not substantively alter treatment choices. Further investigation of the relationships between disease biology, treatment effects, and acquisition/loss of mutations should be conducted in the context of clinical trials. The role of serial mutation profiling in MDS warrants further investigation.
Lee:Boehringer Ingelheim: Consultancy; Baxalta: Consultancy; Amgen: Consultancy; Alexion Pharmaceuticals: Consultancy; Pfizer Inc: Consultancy. Steensma:Genoptix: Consultancy; Janssen: Consultancy; Millenium/Takeda: Consultancy; Ariad: Equity Ownership; Celgene: Consultancy; Amgen: Consultancy. Ritchie:Arian: Speakers Bureau; Novartis: Honoraria; Incyte: Speakers Bureau; Pfizer: Honoraria; Celgene: Speakers Bureau. Desai:Boehringer Ingelheim: Consultancy. Komrokji:Boehringer-Ingelheim: Research Funding; Novartis: Consultancy, Speakers Bureau; Incyte: Consultancy; Celgene: Membership on an entity's Board of Directors or advisory committees, Research Funding. Sekeres:Millenium/Takeda: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees. Roboz:Cellectis: Research Funding; Agios, Amgen, Amphivena, Astex, AstraZeneca, Boehringer Ingelheim, Celator, Celgene, Genoptix, Janssen, Juno, MEI Pharma, MedImmune, Novartis, Onconova, Pfizer, Roche/Genentech, Sunesis, Teva: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal