Abstract

Background
Bendamustine/rituximab (BR) and dexamethasone/rituximab/cyclophosphamide (DRC) combination therapy are acceptable options for the treatment of WM, both in the frontline or salvage setting. Prospective data, however, are only available in treatment-naïve (TN) WM patients, and no direct comparison between BR and DRC has been reported. We compared outcomes of BR and DRC in relapsed/refractory (R/R) and TN WM patients seen at a single institution.
Methods
Records of WM patients seen consecutively at Mayo Clinic from 01/2007 to 12/2014 were reviewed. The MYD88L265P status, as assessed by AS-PCR, was recorded when available. The data obtained from symptomatic patients treated with DRC or BR were analyzed. The time-to-event analyses were performed from DRC or BR therapy using the Kaplan-Meier method. We used the Consensus criteria (6th International Workshop) for response assessment.
Results
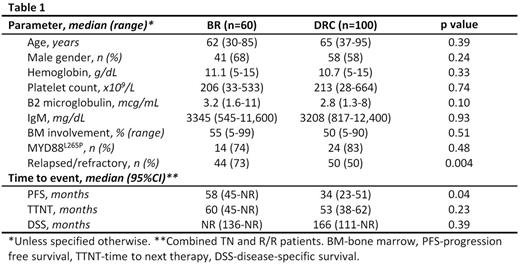
Of 160 WM patients, 60 patients received BR (73% in R/R setting) and 100 patients received DRC (50% in R/R setting). In the R/R population, BR was the 2nd line (range 2-11) therapy in 47% of patients, while DRC was 2nd line (range 2-8) in 58% of patients. Rituximab monotherapy was the only prior line of therapy in 8 (20%) patients in the BR group and 20 (40%) in the DRC group (p=0.66). Baseline characteristics were similar in patients treated with BR or DRC (Table 1). Six patients received both BR and DRC during their disease course and overlapped between the 2 cohorts.
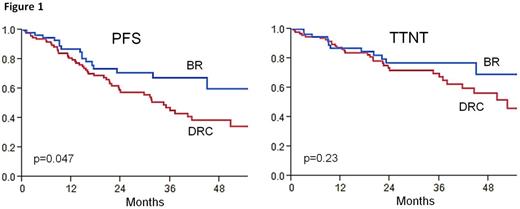
Among the previous untreated patients, the median IgM levels decreased from 3,785 mg/dL to 724 mg/dL (p=0.0001) at best response with BR, while it decreased from 4,130 mg/dL to 1,250 mg/dL (p=0.001) with DRC. The median time to best response was 6.1 (1-25) months in the BR group and 11 (0.5-47) months in the DRC group (p=0.13). For patients treated with BR, the overall response rate (ORR) was 93% [VGPR 29% (n=4), PR 57% (n=8), MR 7% (n=1)]. One patient (7%) had progressive disease. For patients treated with DRC, ORR was 96% [VGPR 17% (n=8), PR 70% (n=32), MR 9% (n=4)]. One patient (4%) achieved SD. Median follow up in the BR and DRC groups were similar (30 months). The 2-year progression-free survival (PFS) was 88% and 61% in the BR and DRC groups, respectively (p=0.08). The 2-year time-to-next therapy (TTNT) was 88% and 76% in the BR and DRC groups, respectively (p=0.35). Median PFS, TTNT and disease specific survival (DSS) were not reached with either regimen.
In the R/R setting, the median IgM levels decreased from 3,880 mg/dL to 659 mg/dL (p=0.0001) at best response with BR, and from 3,870 mg/dL to 1,846 mg/dL (p=0.001) with DRC. The median time to best response was similar [7 (1-39) months with BR and 7 (0.5-28) months with DRC (p=0.77)]. For patients treated with BR, ORR was 95% [CR 3% (n=1), VGPR 38% (n=14), PR 41% (n=15), MR 13% (n=5)]. Two patients (5%) had progressive disease. With DRC, the ORR was 87% [VGPR 4% (n=2), PR 64% (n=30), MR 19% (n=9)]. Four patients (9%) achieved SD and 2 patients (4%) had progressive disease. Median follow up from BR was 32 months and 51 months from DRC (p=0.24). The 2-year PFS was 66% and 53% in the BR and DRC groups, respectively (p=0.08). The 2-year TTNT was 75% and 68% in the BR and DRC groups, respectively (p=0.24). The median DSS in the BR group was 69 months (95% CI: 65-69) and NR (95% CI: NR-NR) in the DRC group (p=0.57).
The proportion of patients with R/R disease was significantly higher in the BR cohort (Table 1). In a bivariate analysis of the entire cohort for PFS, incorporating the setting (TN vs. RR) and the regimen involved (BR vs. DRC), the latter emerged as a significant factor (hazard ratio 0.52, p=0.019) in favor of BR. Time-to-event outcomes and response rates were similar in the MYD88L265P and MYD88WT patients. Grade ≥ 3 adverse events were neutropenia (12%), infections (7%) and nausea/vomiting (2%) with BR, and neutropenia (20%), thrombocytopenia (7%) and infections (3%) with DRC.
Conclusions
Although both DRC and BR regimens show activity and comparable toxicities, BR regimen shows a trend for superior PFS in WM patients, both in the TN and R/R setting. No difference was seen in TTNT. MYD88 L265P mutation status does not appear to impact activity of BR or DRC. Randomized controlled trial(s) are needed to confirm our findings.
Ailawadhi:Pharmacyclics: Consultancy; Novartis: Consultancy; Amgen Inc: Consultancy; Takeda Oncology: Consultancy. Ansell:BMS, Seattle Genetics, Merck, Celldex and Affimed: Research Funding. Reeder:Millennium: Research Funding; BMS: Research Funding; Novartis: Research Funding; Celgene: Research Funding. Dispenzieri:Jannsen: Research Funding; Takeda: Membership on an entity's Board of Directors or advisory committees, Research Funding; pfizer: Research Funding; Prothena: Membership on an entity's Board of Directors or advisory committees; Celgene: Research Funding; Alnylam: Research Funding; GSK: Membership on an entity's Board of Directors or advisory committees. Kumar:Sanofi: Consultancy, Research Funding; Janssen: Consultancy, Research Funding; AbbVie: Research Funding; Array BioPharma: Consultancy, Research Funding; BMS: Consultancy; Kesios: Consultancy; Glycomimetics: Consultancy; Skyline: Honoraria, Membership on an entity's Board of Directors or advisory committees; Noxxon Pharma: Consultancy, Research Funding; Millennium: Consultancy, Research Funding; Onyx: Consultancy, Research Funding; Celgene: Consultancy, Research Funding. Kapoor:Celgene: Research Funding; Takeda: Research Funding; Amgen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal