Abstract
Introduction: Follicular lymphoma (FL) is the second most common type of non-Hodgkin cell lymphoma, and usually manifests as a disseminated disease. Bone marrow (BM) involvement, which occurs in 40-70% of cases, is often seen in follicular lymphoma and thought to be associated with less favorable prognosis. Diagnosis of BM involvement has traditionally been based on morphological findings, and BM involvement has been determined using histology alone in most clinical trials. Immunocytologic or molecular studies, such as flow cytometry (FCM) and polymerase chain reaction (PCR), have become more readily available, and their usage has clearly documented minimal BM involvement reproducibly. In this study, we evaluated the impact of BM involvement detected by FCM and PCR on the outcome of patients treated for FL.
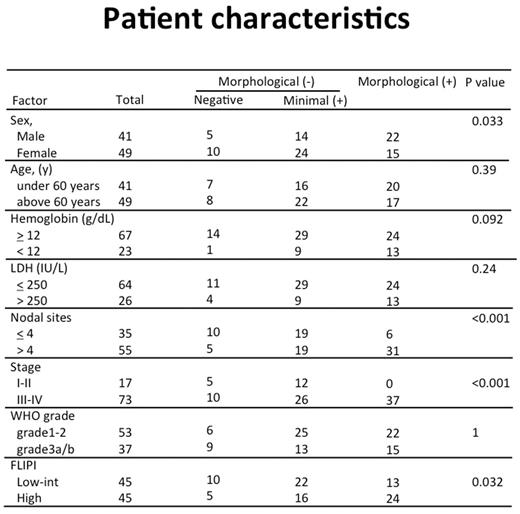
Methods: Patients who were diagnosed with biopsy-proven FL between 2004 and 2015 at our institution were included in the study. All patients had received a staging bone marrow examination before treatment with immunotherapy-based regimen. Immunocytologic [FCM] and/or molecular [PCR] studies were always performed if the patients did not have morphological BM involvement. We used 4- or 6- color FCM, and performed PCR analysis of Bcl-2/IgH rearrangement and/or IgH rearrangement detected by modified BioMed-2 protocol. A total of 90 patients were included, and the median follow-up duration was 36 months (range, 6|122 months). The BM status was classified using into 3 categories: morphological, minimal, and negative BM involvement. Minimal BM involvement was defined as BM involvement detected by FCM or PCR without morphological evidence. Morphological and minimal BM involvements were detected in 37 (41%) and 38 (42%) patients, respectively. The primary outcome measure was progression-free survival (PFS). PFS curves were plotted using the Kaplan-Meier method and compared by the log-rank test. Multivariate analyses were performed using a Cox linear regression model. There were significant differences in gender, LDH levels, stage, nodal sites, and FL International Prognostic Index (FLIPI) between patients with and without morphological BM involvement (Table1).
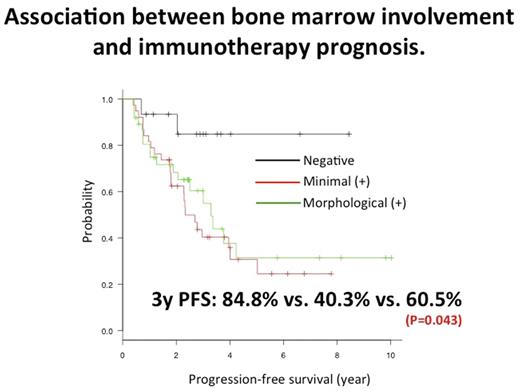
Results: The 3-year PFS rate for patients with negative BM involvement was significantly better than that for patients with minimal or morphological BM involvement (84.8% vs. 40.3% vs. 60.5%; p= 0.043) (Figure 1). There was no statistical difference in 3-year PFS between patients with morphological BM involvement and those with minimal BM involvement. The difference of 3-year PFS rate between patients with minimal BM involvement and those with negative BM involvement was significant for patients with FLIPI low-intermediate risk (88.9% vs. 51.5%; p= 0.032) and those with advanced stage disease (90.0% vs. 33.6%; p= 0.027), but there were no significant differences in patients deemed FLIPI high risk and those with limited stage disease. Multivariate analysis revealed that BM involvement, including morphological and minimal involvement, was a significant poor prognostic factor (hazard ratio 4.885 [95% confidence interval 1.16-20.56], p = 0.0305).
Conclusion: At the start of treatment, bone marrow involvement was seen in most FL patients. Patients without any BM involvement had an excellent prognosis. Patients with minimal BM involvement had an equally poor prognosis as those with morphologic BM involvement.
FLIPI: Follicular Lymphoma International Prognostic Index
BM state positive: including morphological and minimal bone marrow involvement.
BM state positive: including morphological and minimal bone marrow involvement.
Ishikawa:Mundipharma KK: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal