Abstract
Introduction:
Acute myeloid leukemia (AML) is one of the most threatening malignancies in children and adolescents. The accumulation of mutations in leukemia stem cells (LSC) is believed to lead to the development of leukemia. Cyto- and molecular genetics already identified several aberrations which are relevant in leukemogenesis, prognosis and therapy. Nevertheless, the molecular landscape and clonal evolution of AML and its clinical relevance, especially for pediatric patients, is not yet well described. Next Generation Sequencing (NGS) as an emerging sequencing technology provides the possibility to generate sequence data of high quality and detect genetic aberrations in a minimum of time. The aim of this study was to apply amplicon based panel targeted resequencing by using the TruSight Myeloid Panel (Illumina) to identify variants in 54 genes.
Methods
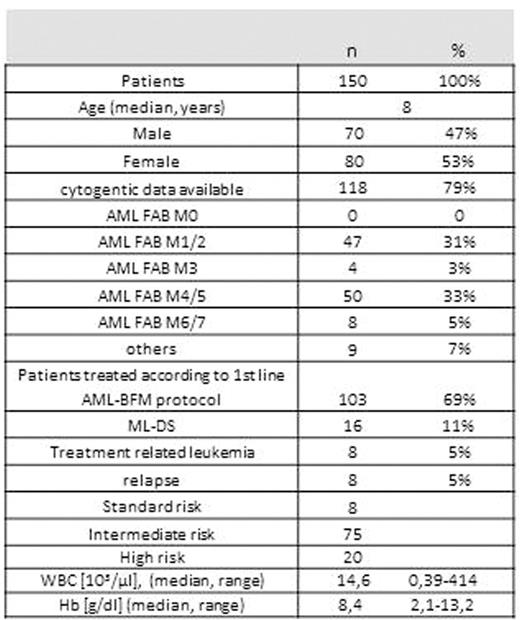
Patients:
In total 150 samples derived from pediatric patients diagnosed with AML at the time of initial diagnosis or relapse were analysed regarding their mutational profile. All patients treated according to the AML-BFM therapy protocols (n=103) were chosen to determine the potential impact in prognosis.
Sequencing and analysis of variants
Sequencing with the TruSight Myeloid panel (Illumina) was performed on a MiseqDX. The sequencing panel is designed to identify somatic mutations associated with myeloid malignancies in 54 genes. To define variants, we excluded intronic, synonymous and variants with an allele frequency below 5% and a read depth below 50 reads. False positive variants were excluded by including healthy donors and reference samples.
Variants were detected and analysed using Variant studio (Illumina) and Sophia DDM (Sophia Genetics). Almost all variants were detectable in both software, although great insertions and deletions were detectable only by Sophia DDM.
Results
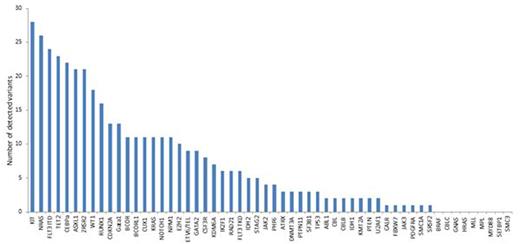
In the cohort of 150 patients, we detected 408 mutations in the 54 genes included in the panel (fig. 1). 26% of the patients showed more than 4, 24% 3, 24% 2, 17% 1 and 9% of the patients showed 0 mutations. Four and more mutations occurred mostly in AML FAB M1 (n=17) and patients with a complex karyotype (n=6). Treatment related AML show less mutations compared to primary AML.
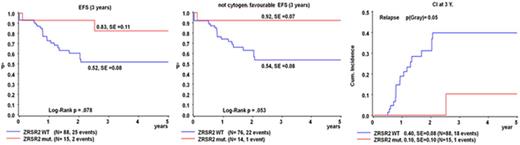
Within the group of patients treated according the 1st line AML-BFM protocol (n=103), CEBPA, FLT3, KIT, NRAS, KRAS, NPM1 or WT1 mutations did not have prognostic relevance. Interestingly, we were able to detect mutations in ZRSR2 in 21 patients in total (SNVs in 6, InDels in 9 and splice acceptor variants in 6 patients). 15 patients were part of the group of patients who were treated according to the 1st line AML-BFM protocol. ZRSR2 encodes an essential splicing factor and the encoded protein associates with the U2 auxiliary factor heterodimer and may play a role in network interactions during spliceosome assembly [RefSeq 2008]. The presence of a ZRSR2 mutation seems to be associated with better EFS and lower cumulative incidence of relapse, respectively (fig.2). Even if patients with favourable cytogenetics were excluded, patients with mutated ZRSR2 might have better EFS (fig.2).
Conclusions:
Amplicon based panel targeted resequencing with the TruSight Myeloid panel provides the possibility to detect mutations in 54 genes associated to myeloid malignancies within 3 days. This will enable a faster and possible more precise characterisation of pediatric AML, either for risk group stratification or the addition of more specific treatment options. Due to the limited number of patients, the results concerning the prognostic relevance of ZRSR2 need to be confirmed in a larger patient group.
patient characteristics
Number of variants detected in 54 genes
Event-free survival (EFS) and cumulative incidence for relapse for patients showing no mutation (blue) or mutations (red) in ZRSR2.
Event-free survival (EFS) and cumulative incidence for relapse for patients showing no mutation (blue) or mutations (red) in ZRSR2.
Reinhardt:Jazz Pharma: Other: Travel Accomodation; Celgene: Research Funding; Celgene: Membership on an entity's Board of Directors or advisory committees; Pfizer: Membership on an entity's Board of Directors or advisory committees; Boehringer Ingelheim: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal