Abstract
<Introduction>
Since an excellent outcome was observed in a previous study (OCLSG-94) utilizing continuous cytarabine (CA) infusion in the consolidation phase for the treatment of pediatric B cell precursor acute lymphoblastic leukemia (BCP-ALL), a randomization trial was performed to test the superiority of continuous CA infusion to conventional repeated CA injection as consolidation therapy in Japan Association of Childhood Leukemia Study (JACLS) ALL02 clinical trial.
<Patients and Methods>
Newly diagnosed children with standard-risk (SR) or high-risk (HR) BCP-ALL excluding patients with Ph+ ALL and infants were included in this study. Patients showing prednisolone good response (PGR) were assigned to SR or HR based on the age at onset and initial white blood cell (WBC) counts (SR: age 1 to 9 and WBC less than 10,000 /µL, HR: remaining patients). Patients achieving complete remission (CR) at the end of induction (day 33) proceeded to the randomization. HR patients with M3 marrow on day 15 were excluded. They were randomly assigned to Arm A (cyclophosphamide 750 mg/m(2) 1hr div: day 1 and 8, CA 75 mg/m(2) 1hr div: day 1-6, 8-13 and 6MP 50 mg/m(2) orally, day 1-14) or Arm B (cyclophosphamide 500 mg/m(2) 1hr div: day 1, 3 and 5, CA 100 mg/m(2) 24hr div: day 1-5 and DEX 5 mg/m(2) 1hr div twice a day, day 1-5). Intrathecal chemotherapy (MTX, HDC and CA) was administered twice in this phase in both arms. In the HR group two doses of pirarubicin (25 mg/m (2)) were added and this phase was repeated after re-induction therapy. Estimation of event free survival (EFS) and overall survival (OS) was performed using the Kaplan-Meier method and the differences were compared using the log-rank test.
<Results and Discussion>
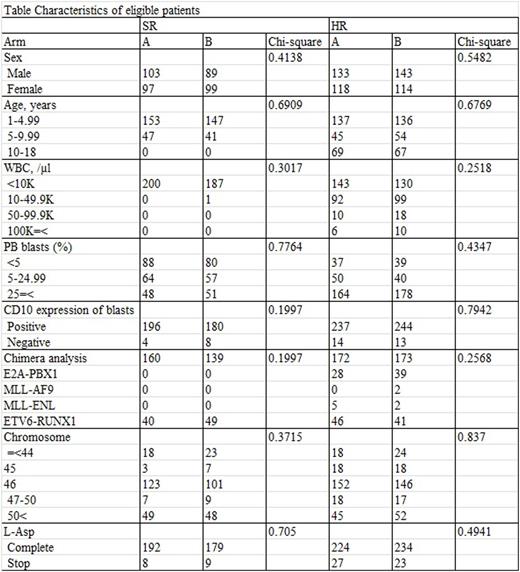
Between April 2002 and May 2008, 1252 children with newly diagnosed ALL were enrolled to JACLS ALL-02 study. Among these, the number of patients with SR and HR were 388 (arm A=200, arm B=188) and 513 (arm A=251, arm B=257, not assigned=5), respectively. The characteristics of eligible patients between arm A and B were not different statistically (Table). Among SR patients, the 4y-EFS were 89.7 +/- 5.2% and 93.4 +/- 4.7% in Arm A and B, respectively (p=0.70). Among HR patients, the 4y-EFS were 89.7 +/- 5.2% and 90.5 +/- 4.4% in Arm A and B, respectively (p=0.97). Although hematological toxicity was not different, in the next phase (sanctuary phase) following Arm A consolidation therapy the frequencies of hematological grade 3 and 4 adverse effects were higher in both SR and HR (SR: p<0.01 in Hb, WBC, and ANC, p<0.05 in Plt; HR: p<0.01 in Hb, WBC, ANC, and Plt). On the other hand, the frequencies of severe adverse effects of liver dysfunction during consolidation phase were higher in Arm B (SR: p<0.05, HR: p<0.01), although grade 3/4 elevation of AST/ALT were not different.
<Conclusions>
Consolidation therapy with continuous infusion of CA (Arm B) was not superior to conventional CA regimen.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal