Abstract
Background: APL is a distinct but rare subtype of acute myeloid leukemia. Once very lethal, the discovery of all-trans retinoic acid (ATRA) as treatment has resulted in high rates of cure. Despite this, early mortality rates remain as high as 10% in clinical trials and may be even higher in general practice, where there may not be significant experience with this uncommon malignancy. Prompt recognition of APL and access to ATRA are critical to preventing early death, which is typically due to hemorrhage-related complications stemming from disseminated intravascular coagulation. We hypothesized that patients treated at teaching hospitals would have lower rates of early mortality as compared to non-teaching hospitals.
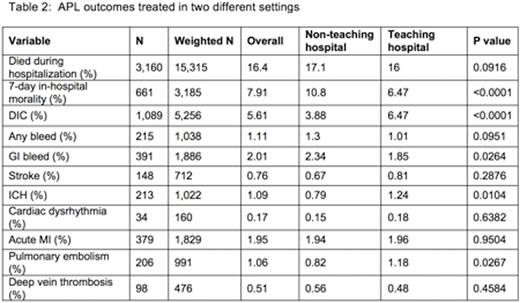
Methods: We queried the Nationwide Inpatient Sample (NIS) from year 2008-2013 to identify patients >18 years of age with a discharge diagnosis of APL based on ICD-9 CM code of 205.00. A survey weighted domain analysis was conducted to describe the relationship between hospital teaching status and clinical outcomes among adult patients. Teaching hospitals have an AMA-approved residency program or have membership in the Council of Teaching Hospitals. Patient characteristics and clinical outcomes (in-hospital mortality, 7-day in-hospital mortality, disseminated intravascular coagulation (DIC), bleeding, stroke, cardiac dysrhythmia, acute myocardial infarction (AMI), pulmonary embolism (PE), deep vein thrombosis (DVT), and length of stay) were compared across hospital teaching status using ANOVA for continuous variables and Chi-squared tests for categorical variables. Multiple logistic regression was used to compare binary outcomes by hospital teaching status adjusting for patient characteristics.
Results: The baseline characteristics of the patients are described in Table 1. Patients at non-teaching hospitals were older (mean age 68 yrs. vs. 60.3 yrs., p<0.0001) and had higher Charlson co-morbidity index (CCI) (mean 3.85 vs. 2.84, p<0.001). Patients treated at teaching hospitals had higher rates of DIC (6.47% vs. 3.88%, p<0.0001), ICH (1.24% vs. 0.79%, p=0.0104), and PE (1.18% vs. 0.82%, p=0.0267). The rate of gastrointestinal bleeding was higher in the non-teaching hospitals (2.34% vs. 1.85%, p=0264). Rates of overall bleeding, AMI, and cardiac arrhythmia were similar between both groups (Table 2). The 7-day in-hospital mortality was significantly higher in non-teaching hospitals, 10.8% vs. 6.47% (p<0.0001), however there was no difference in the overall in-hospital mortality between the two groups (17.1% non-teaching vs. 16% teaching, p=0.09). On multiple logistic regression analysis, treatment at teaching hospital (OR 0.73, 95% CI 0.64-0.82; p<0.001), age (OR 1.03, 95% CI 1.03-1.04; p<0.001), female sex (OR 0.84, 95% CI 0.76-0.94; p=0.003) and CCI (OR 1.5, 95% CI 1.35-1.76; p<0.001) had significant impact on the 7-day in-hospital mortality (Table 3).
Conclusion: Our analysis from the large NIS database showed that the early in-hospital mortality in patients with APL was significantly higher in patients treated at non-teaching hospitals as compared to teaching hospitals. Patients treated at teaching hospitals had better outcomes despite higher rates of DIC, ICH, and PE. The overall rate of death during initial hospitalization was higher than what is typically reported in clinical trials but there was no difference between the two hospital settings. The lower rate of early hospital mortality in teaching hospitals may be attributable to early recognition and initiation of ATRA therapy due to clinician experience. Thus, efforts should be made to increase awareness of APL in the non-teaching hospital setting so that prompt treatment and appropriate referral can be considered if needed.
Michaelis:Pfizer: Equity Ownership; Cellgene Corporation: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Incyte Corporation: Consultancy, Honoraria. Hamadani:Janssen: Consultancy; Celgene: Honoraria, Research Funding; Takeda Pharmaceuticals: Research Funding. Fenske:Millennium/Takeda: Research Funding; Seatle Genetics: Honoraria; Celgene: Honoraria; Pharmacyclics: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal