Abstract
Background: The effectiveness and safety of acute venous thromboembolism (VTE) treatment with rivaroxaban, demonstrated in phase-III trials, needs to be evaluated in unselected patients treated under daily care conditions.
Patients and methods: The Dresden NOAC registry is a prospective regional registry in which patients with oral anticoagulation undergo prospective follow- up (FU). So far, more than 3200 patients have been enrolled, including 772 VTE patients with rivaroxaban treatment. For this analysis, only patients with acute VTE who started rivaroxaban within 14 days after diagnosis of VTE and who were enrolled within these 14 days were evaluated with regard to patient characteristics, treatment persistence and clinical outcomes. All reported outcome events were centrally adjudicated based on source documentation and standard definitions.
Results: Between December 1st 2011 and March 31st 2016, 407 patients received rivaroxaban for acute VTE treatment (51.6% female, 80.8% DVT; 19.2% PE±DVT, mean age 61.4 years). Mean time between VTE diagnosis and initiation of rivaroxaban was 1.7±3.3 days (median 0d; 25th/75th percentile 0; 1d). At baseline, rivaroxaban doses consisted of 15 mg BID in 93.1%, 20 mg OD in 3.4%, 15 mg OD in 3.2% and 10 mg OD in 0.2% of patients. Reasons for not using 2x15 mg rivaroxaban BID were pre-treatment with therapeutic parenteral anticoagulants for ≥7 d in 14 cases, comorbidities (e.g. bleeding history, renal impairment) in 4 cases and unknown in 10 cases.
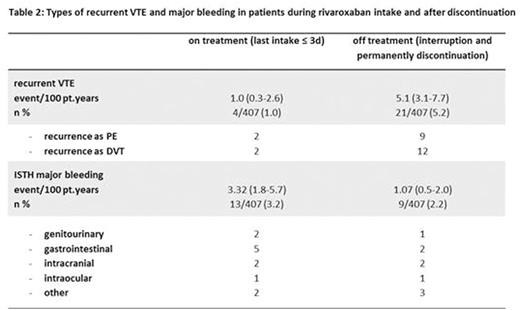
During FU (mean 762.4±462.7d), the mean rivaroxaban exposure was 357.7±385.9 days. During treatment with rivaroxaban, 4/407 patients (1.0%) experienced a recurrent VTE, which translated into a recurrence rate of 1.0/ 100 pt. years.
During treatment, 172/407 (42.3%) patients reported bleeding complications, which in 13 cases (3.2%; 3.3/100 pt. years) were major bleeding according to ISTH definition, including one fatal intracranial bleeding.
Patients with deep vein thrombosis (DVT) and pulmonary embolism (PE) had similar rates of recurrent VTE during rivaroxaban treatment (1.01 and 1.01/100 pt. years) but PE patients had numerically higher rates of major bleeding (3.99/100 pt. years compared to 3.09/100 pt.years in the DVT group).
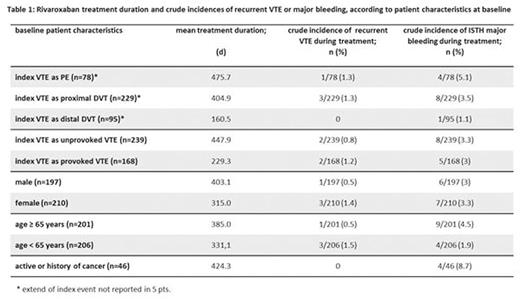
Effectiveness and safety profiles were consistent across relevant subgroups (table 1).
18 patients died during FU (2.12/100 pt.years), of which 8 deaths occurred during or within 3 days after last intake of rivaroxaban. Most common causes of death were fatal cardiovascular event (n=7) and terminal malignant disease (n=4), followed by sepsis/infection (n=3), age related death (n=1), fatal bleeding (n=1) and other reasons (n=2).
At 6 months (FU completed in 365 pts.), 61.4% of patients were still taking rivaroxaban. The remaining patients had a scheduled end of treatment (28.8%) or were switched to other anticoagulants (7.1%). Therefore, the rate of unplanned complete discontinuation at 6 months was 2.7%.
At 12 months (FU completed in 289 pts.), 41.5% of patients were still taking rivaroxaban. The remaining patients had a scheduled end of treatment (45.0%) or were switched to other anticoagulants (8.3%). Therefore, the rate of unplanned complete discontinuation at 12 months was 5.2%.
After rivaroxaban interruption for more than 3 days or permanent discontinuation, 21 patients experienced a recurrent VTE (9 PE±DVT, 12 DVT) with a mean time between last intake of rivaroxaban and VTE recurrence of 351.2±282.6 days (range 7-926d). PE was a common manifestation of VTE recurrence and, despite numerically lower bleeding rates after discontinuation, 2 cases of intracranial haemorrhage occurred (table 2).
Conclusions: In unselected patients in daily care, rivaroxaban treatment for acute VTE has high effectiveness and acceptable rates major bleeding. Initial dosing was according to label in over 90% of patients and, at 6 and 12 months, persistence to rivaroxaban therapy was excellent with low rates of unplanned complete discontinuation. Fatal VTE and fatal bleeding are rare events during rivaroxaban therapy and all-cause mortality is mostly related to underlying diseases, age or acute co-morbidities. Treatment discontinuation resulted in a relevant increase in VTE recurrence, of which more than 40% manifested as PE. In contrast, major bleeding rates declined after discontinuation but with 1%/year remained at a clinically relevant level, probably due to co-morbidities.
Marten:Bayer: Honoraria; Daichii Sankyo: Honoraria. Werth:Pfizer: Honoraria; Bayer: Honoraria; Boehringer Ingelheim: Honoraria; Daiichi Sankyo: Honoraria; OmniaMed: Honoraria; LEO-Pharma: Honoraria. Beyer-Westendorf:Pfizer: Consultancy, Honoraria, Research Funding; Boehringer Ingelheim: Consultancy, Honoraria, Research Funding; Daichii Sankyo: Consultancy, Honoraria, Research Funding; Bayer: Consultancy, Honoraria, Research Funding; LEO: Consultancy, Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal