Abstract
Background:
The characteristics of post-surgical thrombocytopenia have not been well described. Interpretation of the reported data was potentially confounded by the fact that many of the patients were receiving heparin.1,2
We aimed to evaluate the post-operative thrombocytopenia in orthopedic surgery patients who were not exposed to heparin in order to better define the characteristics of this phenomenon.
Methods:
A retrospective chart review was conducted on patients who underwent a knee or hip replacement from 2012 to 2015. Exclusion criteria were: age <18, pre-op platelet count (PLT): <150 or > 400 (x10^9/L) or heparin exposure.
Results:
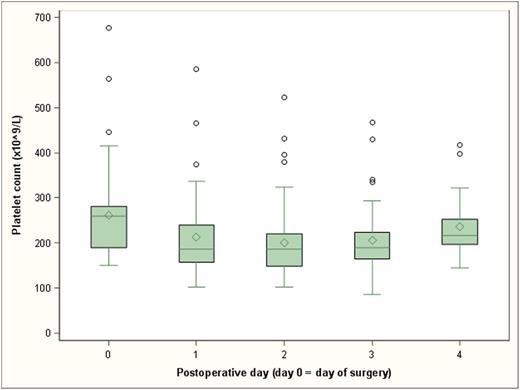
A total of 56 patients were analyzed on post-op days 0 to 4. One patient had missing data at day 1 and was not included in final analysis. By day 1, 51 patients experienced a reduction in PLT (92.7%). The lowest mean PLT (nadir) occurred at day 2 (mean=201.3x10^9/L). The average decrease in PLT between baseline and nadir was 24% (95% CI: 20.6-27.2). The change in PLT between baseline and nadir ranged from a 49.6% drop to a 14.2% increase (see Figure 1).
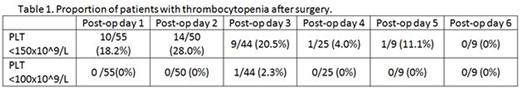
A substantial portion of patients experienced thrombocytopenia, defined as a PLT less than 150x10^9/L, with 28% occurring on day 2 as shown in Table 1. However, more severe thrombocytopenia with PLT less than 100x10^9/L occurred in only one patient.
The highest mean WBC count occurred at day 1 (mean=11.0x10^9/L) with an average increase of 16.1% (95% CI: 5.8-27.6) relative to baseline.
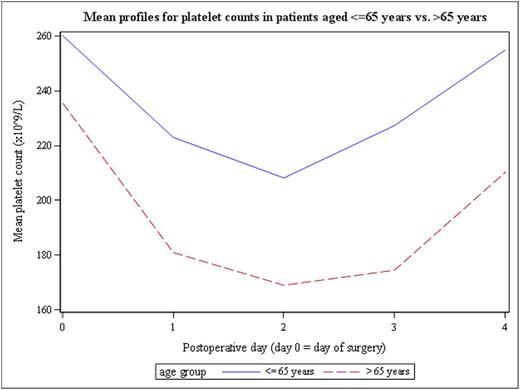
We analyzed the association between PLT and other factors. Mean PLT were significantly lower (on average 24.8x10^9/L lower, 95% CI: 8.7-40.9) at days 1 to 4 in patients aged >65 years, compared to patients aged ≤65 years (p=0.004) as shown in Figure 2. Specifically, the average drop in PLT at nadir (day 2) relative to baseline was significantly larger in patients aged >65 years (mean PLTday2 - mean PLTday0 = -72.3x10^9/L) compared to patients aged ≤65 years (mean PLTday2 - mean PLTday0 = -47.5x10^9/L.
Discussion:
Our data demonstrate that reduction in PLT occurs frequently after orthopedic surgery in a non-heparinized population. This drop was seen in the majority of patients (92.7%) with the nadir occurring on day 2, as previously published.1,2 However, only 28% of patients were actually thrombocytopenic. In addition, five patients had an increase in PLT by day 1 without any significant drop below baseline thereafter. There was no significant association with regards to age, gender, or type of surgery to explain this rise in PLT.
This study also highlighted several other points which have not previously been published in the literature. There was a significant difference in PLT reductions in patients >65 years compared to ≤65 years (24.8x10^9/L), suggesting that advanced age increases the risk of thrombocytopenia which requires closer monitoring.
The etiology for the decreased PLT cannot be bone marrow suppression, since there was no concordant decrease in WBC count. The rise in WBC count suggests an inflammatory response that should have been reflected in a secondary thrombocytosis. This discrepancy is unexplained.
Although 28% of patients experienced thrombocytopenia by day 2, the nadir remained >100x10^9, and only one patient had PLT below that level. Therefore, alternative causes should be considered in patients that experience severe thrombocytopenia post-operatively, as this was a rare finding in our study.
Conclusion:
Reduction in PLT is a frequent post-operative finding in orthopedic surgery patients, even after removing confounding factors such as heparin exposure, but clinical thrombocytopenia is uncommon. Nadirs typically occur by day 2. Alternative etiologies should be considered when PLT is <100x10^9/L. Vigilance should also be considered with regards to elderly patients as age >65 was associated with a more significant drop in PLT post-operatively.
References:
1. Warkentin TE. Thrombocytopenia Caused by Platelet Destruction, Hypersplenism, or Hemodilution. In: Hoffman R, Benz EJ, Silberstein LE, Heslop HE, Weitz JI, editors. Hematology: Basic Principles and Practice, ed 6. Elsevier Inc.; 2013. p. 1895-912.
2. Greinacher A, Selleng K. Thrombocytopenia in the intensive care unit patient. Hematol Educ Program Am Soc Hematol Am Soc Hematol Educ Program 2010;2010:135-43.
Post-operative platelet count profiles in patients aged <=65 years vs. > 65 years.
Post-operative platelet count profiles in patients aged <=65 years vs. > 65 years.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal