Abstract
Background: Patients with idiopathic thrombocytopenia exhibit striking heterogeneity in bleeding manifestations even at similar platelet counts. Proposed mechanisms are generation of platelet microparticles, complement activation, NO depletion, and impact of various treatment modalities. In the present study, we studied the prevalence of thrombophilic markers in persistent and chronic ITP patients and that whether the presence of such markers modifies the clinical course of these patients.
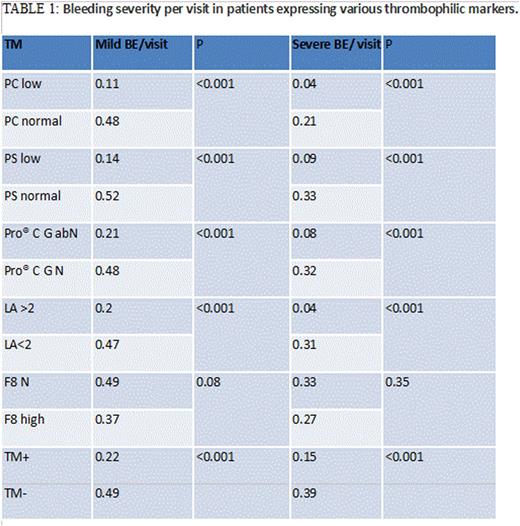
Methods: Patients diagnosed as persistent or chronic ITP (of any age group) were eligible. All patients were evaluated at baseline and at regular follow-up visits using newly available Bleeding Assessment Tool (ITP-BAT, version 1.0) proposed by International Working Group on ITP. For analyses, severity of bleeding was defined as no bleeding (bleeding score zero at all domains I.e. skin, mucosa and organ), mild bleeding (skin and mucosal bleeding score 0-2, organ bleeding score 0-1) and severe bleeding (skin and mucosa bleeding score >2, and organ bleeding score >1). Baseline thrombophilia profile was obtained for all patients, that included clot-based assays for protein C (PC), protein S (PS), ProCGlobal, FVIII levels (F8), and lupus anticoagulant assay (LA). We then compared the patients expressing atleast one thrombophilia marker (TM+) and those without (TM-), for the number of times patients in each group presented with a bleeding episode. We derived the parameter bleeding episodes per visit to estimate severity of bleeding in each group [mild bleeding episode/visit (MBE/visit) and severe bleeding/visit (SBE/visit)].
Statistical analysis was done using odds ratio calculation and correlation regression analysis.
Results: Of the total 88 patients enrolled, 21 were males (23.4%), and remaining 67 (76.5%) were females. Out the total, 57 patients (64.7%) tested positive for at least one thrombophilic marker, and remaining 31 patients (35.2%) were negative for all markers. Raised factor VIII was found in 36 patients (40.9%), low protein S in 29 patients (32.9%), low protein C in 14 patients (15.9%), abnormal Pro® C global in 22 patients (25%), and lupus anticoagulant positive in 9 patients (10.2%). Thirty three (37.5%) patients expressed thrombophilic markers in various combinations. Evaluation for impact of thrombophilia marker on bleeding is as shown in Table 1.
Summary: Sixty-five percent of patients had thrombophilia marker positive in various combinations. Those with thrombophilia had lower bleeding tendency compared to those with none. Patients with low protein C and S, abnormal ProcGlobal and lupus positivity had significantly lower bleeding tendencies, while FVIII abundance did not impact the bleeding scores.
Conclusion: We conclude that a part of the heterogeneity in the clinical presentation of persistent and chronic ITP can be explained by the presence or absence of thrombophilia, and that work-up of patients with ITP should include thrombophilia evaluation, the results of which may have a role in therapeutic decision making.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal