Introduction: Recently, there has been general interest in using marijuana as an analgesic for various types of pain. Cannabis is known to relieve severe nausea and vomiting. Anecdotally, medical marijuana has analgesic effects in patients with chronic and neuropathic pain other than sickle cell pain, decreases the frequency of migraine headache, has anti-spastic effect in multiple sclerosis, and may relieve some of the signs and symptoms of amyotrophic lateral sclerosis and Crohn's disease. Its role in epilepsy is controversial. On the negative side long-term cannabis use is associated with periodontal disease, maternal marijuana use at 20 weeks gestation was strongly associated with spontaneous pre-term birth independent of maternal cigarette smoking and illegal synthetic cannabinoids (K2/spice) were associated with catatonia and myocardial infarction in adolescents. Studies in the transgenic sickle cell mouse showed that cannabinoid receptor-specific mechanisms ameliorate pain via inhibition of mast cell activation and neurogenic inflammation. A questionnaire study from the United Kingdom showed that 36% of the patients with sickle cell disease (SCD) have used cannabis in the previous 12 months to relieve symptoms. Another longitudinal questionnaire study in Jamaica found that marijuana was not related to the clinical severity of SCD. The objective of this study is to report the epidemiological and clinical features of the patients with SCD who were found to be taking marijuana by using random urine drug screening from 1994 to 2009. The frequency of vaso-occlusive crises (VOCs) in these patients was compared to patents with SCD whose urine drug screening showed no marijuana. The terms marijuana and cannabinoid will be used interchangeably in this Abstract.
Patients & Methods: A total of 270 random urine drug screen tests were done on 72 patients representing 10% of our patients with SCD during the period of the study. Written consent was obtained from the patients for enrollment in the study that was approved by the IRB. Types of SCD were determined by routine lab tests. Urine samples, collected randomly, were analyzed for the presence of amphetamine, benzodiazepines, opiates, barbiturate, cannabinoid, propoxyphene, methadone and phencyclidine. Samples were classified as either positive or negative for cannabinoid. Statistical analysis included the two-tailed student's t, Fisher exact and the Chi Square tests.
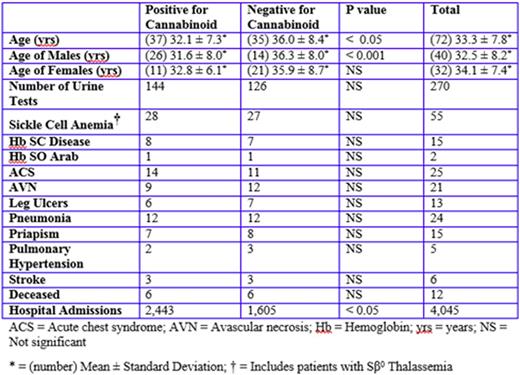
Results: Thirty-seven of the 72 patients tested positive for cannabinoid in their urine and 35 patients tested negative. Table 1 shows the major epidemiological and clinical feature of the patients studied. There was no significant difference in ages of men and women who used or did not use marijuana (p > 0.05). However, males who used marijuana were significantly younger (p < 0.001) than males who did not (Table 1). Moreover, the ages of females who tested positive for cannabinoid were not significantly different from women who tested negative (Table 1). The patients who tested positive for cannabinoids also tested positive for other illicit drugs more often than patients who tested negative. Positivity for benzodiazepines, cocaine and phencyclidine were significantly higher in patients who used marijuana than the nonusers. Notably, there was no significant difference in the use of opioids consumed by users and non-users of marijuana. Similarly, there was no significant difference in the frequency of complications of SCD between users and non-users of marijuana (Table 1). The most important aspect of the study is the effect of marijuana use on the frequency of utilization of medical facilities. Patients in the marijuana cohort were admitted to the hospital for VOCs more frequently (Table 1) than the control group: 2,443 versus1,602 admissions respectively (p < 0.05).
Conclusion: Together these data suggest that patients in the marijuana cohort were more often in severe pain that required treatment in the hospital for VOCs than non-users. This difference could be due to the quality of the marijuana used, the neuronal effects of marijuana and the severity of pain in the users of marijuana. The role of marijuana in the treatment of sickle cell pain seems more complex than thought. Further controlled trials are needed to clarify this issue.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal