Abstract
Background
Transcranial Doppler (TCD) ultrasonography is the standard stroke screening test for children with sickle cell anemia (SCA). However, approximately 10% of children have inadequate ultrasonographic windows for a successful TCD study, and some clinical sites may lack the equipment or personnel to perform TCDs in children. Magnetic resonance imaging (MRI) techniques can also measure blood flow velocities and could substitute for TCD in these clinical scenarios. We tested the hypothesis that MRI-derived middle cerebral artery (MCA) blood flow velocities would correlate with TCD-derived MCA blood flow velocities in children with SCA.
Methods
Children age 6 years and up with SCA at their baseline state of health underwent TCD and MRI as part of a prospective clinical study. Imaging TCD of the bilateral MCAs to determine time-average mean of maximum blood flow velocities (TCD-CBFV) were performed using clinical ultrasound equipment. MRIs were performed at 3T without sedation. MRI cerebral time-averaged mean blood flow velocities (MR-CBFV) were measured in the MCAs using phase contrast sequences without cardiac cycle gating to shorten acquisition time and reduce ghosting artifacts. TCD- and MR-CBFV of each hemisphere were compared. Silent cerebral infarctions (SCIs) were categorized as present or absent in each hemisphere. Non-parametric tests were used with a level of significance of <0.05. Statistics were performed in SPSS version 21.
Results
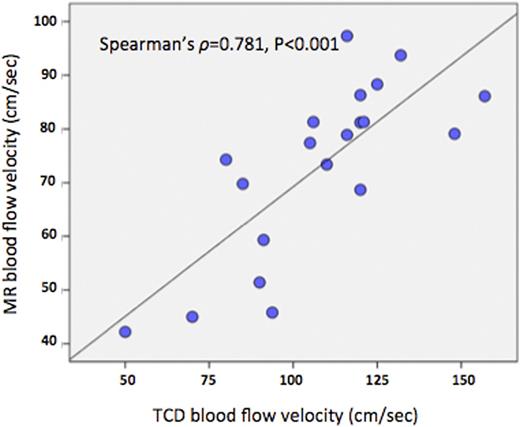
Twenty hemispheres from 15 children had both TCD-CBFV and MR-CBFV measurements. Median age was 9 years (IQR 6.25-10). In these children, two hemispheres had unobtainable TCDs due to skull thickness, and eight hemispheres had MR-CBFV excluded due to patient motion or poor positioning. The median TCD-CBFV was 116 cm/sec (IQR 90.25-124) and none of the included hemispheres had arterial stenosis or TCD-CBFV in the conditional or abnormal range. Eight included hemispheres were from children receiving chronic blood transfusion therapy for primary or secondary stroke prevention. There was a linear relationship between TCD-CBFV and MR-CBFV (Spearman correlation, ρ=0.781, p<0.001, Figure) although MR-CBFV values were lower than TCD-CBFV values (median difference 32.6%, IQR 26.7-42.8). When evaluating only the children not receiving chronic transfusion therapy, MR-CBFV was significantly higher in 8 hemispheres without SCIs (median 80 cm/sec, IQR 77.8-87.8) than in 4 hemispheres with SCIs (median 60 cm/sec, IQR 44.6-72.3, p=0.004). In a multivariate model adjusting for age, MR-CBFV continued to be associated with presence of SCIs (p=0.036). There was no significant difference in TCD-CBFV when analyzed by SCI status (p=0.2), consistent with published studies of TCD-CBFV and SCIs.
Conclusions
In this small cohort of children with SCA, MR-CBFV correlated significantly with TCD-CBFV, but MR-CBFV values were approximately 30% lower than TCD-CBFV. This may be due to the method of acquiring MR-CBFV via non-gated methodology, which is known to produce lower blood flow velocity estimates. Further work is needed to determine a threshold for high-risk MR-CBFV values before this modality could be used as a substitute for TCD screening. Lower MR-CBFV was associated with SCIs, suggesting a potential role for MR-CBFV in predicting SCI risk. The relationship between MR-CBFV and SCIs should be explored further.
Hulbert:Pfizer, Inc.: Other: spouse employment. Fields:NeuroPhage Pharmaceuticals: Equity Ownership, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal