Abstract

Background: Sickle cell disease (SCD) is a life-threatening genetic disease whose patients suffer from chronic anemia, hemolysis, vascular damage, and impaired cerebral blood flow that lead to early and cumulative neurological insults. Adverse effects associated with chronic anemia and hemolysis in SCD include progressive large vessel vasculopathy, stroke, silent cerebral infarctions, and ultimately, early mortality. Few studies have attempted to characterize the effects of this disease on brain morphometry and most have been limited to school age children, despite the progressive nature of the cerebrovascular disease. Thus, this study aims to quantify the hematological effects of SCD on brain morphometry in adolescents and young adults.
Methods: 3D T1-weighted images (TE =3.8ms TR =8.3ms; resolution = 1mm3) were acquired on 25 clinically asymptomatic SCD patients (age=20.8 ± 6.7; F=13, M=12) and 26 ethnically matched control subjects (age=26.4 ± 7.7; F=17, M=9). MRI data were acquired on a 3T Philips Achieva (v.3.2.1) using an 8-channel head coil. All patients were recruited with informed consent or assent; the study was approved by the Institutional Review Board at Children's Hospital Los Angeles (CCI#11-00083). Exclusion criteria included pregnancy, previous overt stroke, acute chest, or pain crisis hospitalization within one month.
T1-weighted images were processed using BrainSuite (brainsuite.org) in a semi-automated fashion to calculate whole brain gray matter volume (GMV), and white matter volume (WMV). Stepwise multivariate regression analysis was run on GMV and WMV against laboratory data and vital signs to find predictors of total brain volume. Laboratory data probed including complete blood counts and indices, quantitative hemoglobin electrophoresis, and markers of hemolysis (LDH, reticulocyte count, cell free hemoglobin). After correcting for age and sex, the remaining predictors of grey and white matter volume were used to probe for regional changes in brain volume through tensor based morphometry (Brain Suite Statistics Toolbox).
Results: White matter, but not grey matter, was diffusely smaller in SCD patients. Sex, age (log transformed) and mean platelet volume (MPV) were the parameters retained in the multivariate model to predict GMV (r2=0.65; F ratio=28.9) where MPV had a positive correlation to GMV. Hemoglobin, sex, and MPV were found as predictors of WMV (r2=0.43; F ratio = 11.8) where both hemoglobin and MPV had a positive correlation to WMV.
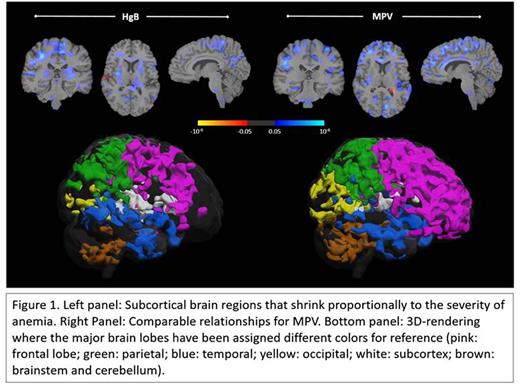
Using tensor based morphometry (TBM), both hemoglobin and MPV were positively associated with brain volume changes diffusely in the frontal, parietal, and temporal cortices (Figure 1). Hemoglobin had a strong localized effect on the subcortex (white matter and basal ganglia) (Figure 1) suggesting that anemia was associated with volume loss in these areas. MPV overall was found to have a strong effect on cortical morphology diffusely.
Conclusion: Hemoglobin's relationship to brain volume and morphology suggests global white matter shrinkage due to anemia. The association is strongest in the phylogenetically younger portions of the brain and co-localizes with brain regions impacted by silent stroke. MPV was an unexpectedly strong predictor of cortical volumes in both SCD and control subjects. MPV is an indicator of platelet activation and is associated with ischemic stroke, hypertension, obstructive sleep apnea, and coronary artery syndromes in the general population, similar to C-reactive protein. However, the broad association of MPV and grey matter volumes in both SCD patients and controls, independently, suggests a developmental interplay between brain maturation and inflammatory signaling that requires further study.
Wood:Celgene: Consultancy; Ionis Pharmaceuticals: Consultancy; AMAG: Consultancy; Apopharma: Consultancy; Apopharma: Consultancy; Biomed Informatics: Consultancy; Biomed Informatics: Consultancy; AMAG: Consultancy; Celgene: Consultancy; Vifor: Consultancy; Ionis Pharmaceuticals: Consultancy; World Care Clinical: Consultancy; Vifor: Consultancy; World Care Clinical: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal