Abstract
Background A recent retrospective study compared healthcare outcomes and costs in pts with MM receiving CAR or POM using health insurance claims data and reported that CAR pts had higher healthcare costs than POM pts (Parikh ASCO 2016). The results of this analysis have not been confirmed by other investigators.
Objective To compare HRU and costs among pts receiving monotherapy with CARor POM +/-dexamethasone (dex) as 2nd or subsequent Tx for MM in the US using a health insurance claims database.
Methods This was a retrospective observational study using the MarketScan® database. Pts were adults with MM (ICD-9-CM code 203.0) who initiated MM Tx, including CAR, POM, bortezomib, lenalidomide, thalidomide, and other chemotherapies (CT) for MM, between Jan 1, '06 and Dec 31, '14. Pts were excluded for (1) Receipt of a MM Tx before the first MM diagnosis date (Dx date) (2) enrollment gap during the 180-days before Dx date, or between Dx date and the first day on Tx, or the 30 days after Tx initiation, or (3) age <18 y at Tx initiation.
Medical/pharmacy claims for MM Tx including CT were tracked for each pt since Tx initiation. After initiation of a first treatment, subsequent lines of therapy (LOT) were identified based on evidence of a new Tx after 90 days since LOT initiation, or >90-day gap in Tx. For each pt with ≥1 CAR or POM LOT, the first LOT with CAR or POM was defined as the index LOT. The date of initiation of this LOT was defined as index date. Pts with CAR or POM as 1st line Tx or in combination with other CT (excluding dex) or with stem cell transplant (SCT) during the index LOT were excluded. Monthly HRU and costs during the index LOT (total, on Tx, off Tx) were compared for pts receiving monotherapy (+/- dex) with CAR vs. POM using inverse probability of treatment weights (IPTW) to obtain average treatment effect (ATE) estimates controlling for measured baseline covariates. IPTWs were based on propensity scores for receipt of CAR estimated by logistic regression with LOT, age, sex, region, plan type, Charlson index, comorbidities, pre-index healthcare cost, and receipt of prior SCT as covariates.
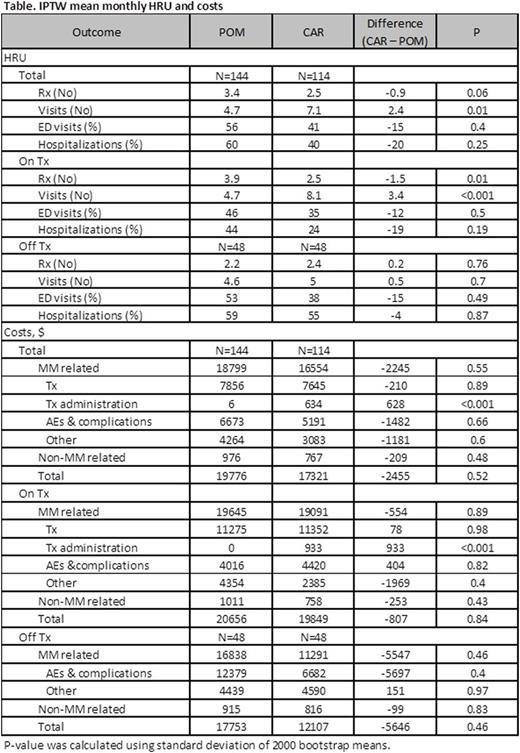
Results We identified 114 CAR and 144 POM pts. CAR pts were more likely to receive index Tx in 2nd vs. subsequent LOT, initiate LOT after 2013, be male, and have chronic renal disease, anemia, and diabetes. POM pts were more likely to have prior SCT, chronic pain, and coronary heart disease. Based on examination of standardized differences, IPTW samples were well balanced in baseline characteristics. IPTW adjusted mean monthly total healthcare costs were $19,776 with POM vs. $17,321 with CAR (difference=-$2,455, p=0.52) (Table). Consistent with its mode of administration, the adjusted mean monthly numbers of visits and costs of Tx administration were greater for CAR. The adjusted mean monthly number prescriptions (Rx) were greater for POM vs. CAR. Otherwise, there were no statistically significant differences between groups in adjusted mean monthly total HRU and costs.
Conclusions IPTW-adjustedmonthlyHRU and costs do not vary significantly for pts receiving monotherapy with CAR or POM +/- dex for 2nd or subsequent line Tx for MM. To avoid potential bias, treatment comparisons using real world evidence require consideration of patient characteristics that may influence treatment choices and outcomes.
Panjabi:Amgen, Inc.: Employment, Equity Ownership. Hagiwara:Amgen, Inc.: Research Funding. Delea:Amgen, Inc.: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal