Abstract
Introduction:
In curable malignancies, early mortality can significantly contribute to poor outcomes, particularly in older patients with comorbidities. Prior studies have demonstrated an association between survival, and health system and socioeconomic factors.
The aim of this study was to analyze the association between such factors and 30-day mortality of patients diagnosed with DLBCL.
Methods:
This was a retrospective study that utilized the National Cancer Data Base (NCDB) to identify patients with DLBCL diagnosed between 1998 and 2012. Patients with complete data for sex, age, race, education, income, distance traveled for health care, hospital type, facility location, urban/rural, insurance, Charlson co-morbidity score, chemotherapy use, time from diagnosis to treatment initiation, use of hematopoietic stem cell transplant, 30 day mortality, last contact, and vital status were included. Chi-square test was used to examine the association between 30-day mortality and categorical variables. Multiple logistic regression model was used for multivariate analysis.
Results:
The study population included 51,119 individuals. Characteristics included a median age of 66 years, 92% whites and 47% females. The risk of 30-day mortality was 3.4% for the entire cohort. In a univariate analysis, female versus male sex (3.1% vs 3.4%, p=0.02), urban versus rural location (3.2% vs. 5.3%, p<0.001), lower Charlson comorbidity scores (2.3% vs.5.1% vs. 10.8% for scores of 0, 1 and 2 respectively, p<0.0001), and age ≤60 years versus >60 years (1.5% vs 4.4%, p<0.001) were associated with a lower 30-day mortality.
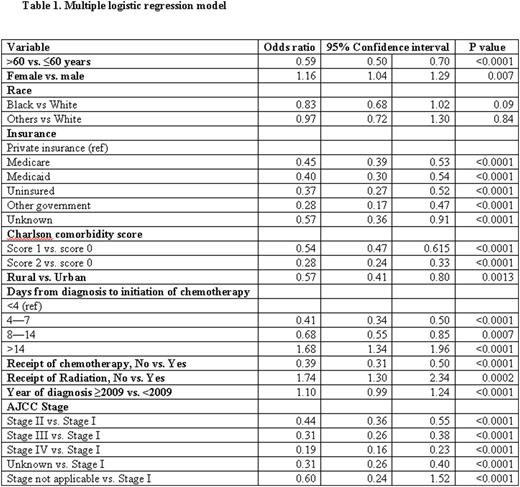
In a multivariate analysis, females, compared to males, were more likely to be alive at 30 days (odds ratio, OR 1.16, 95% confidence interval, CI 1.04-1.29) (Table 1). Uninsured patients (OR 0.37, 95% CI 0.27-0.51) and patients with Medicare (OR 0.45, 95% CI 0.39-0.53), Medicaid (OR-0.40, 95% CI 0.30-0.54), and other government insurances (OR-0.28, 95% CI 0.17-0.47), compared to those with private insurance, had lower likelihood of surviving at 30 days. People from rural areas had a lower 30-day survival rates when compared to urban areas (OR-0.72, 95% CI 0.41- 0.80). Higher Charlson comorbidity, older age, higher AJCC stage were associated with lower 30-day survival rates. The 30-day survival did not differ with the race, annual income, level of education and type of treating facility.
Conclusion:
The 30-day mortality in patients with DLBCL depends not only on biologic factors such as age, comorbidities, and stage, but also on health system and socioeconomic factors such as gender, type of insurance, and location of the hospital. Further investigations into such factors contributing to the increased mortality may help reduce the gap in outcomes.
Armitage:ZiopharmOncology: Consultancy; GlaxoSmithKline IDMC: Consultancy; Spectrum Pharmaceuticals: Consultancy; Roche: Consultancy; Conatus - IDMC: Consultancy; Tesaro bio Inc: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal