Abstract
Introduction
Allogeneic transplantation from a haploidentical donor (HaploSCT) is an alternative strategy in the treatment of hematologic malignancies in absence of HLA-identical donor. Recent studies reported similar outcome after HaploSCT compared to HLA-identical transplantation in different settings (Bashey, JCO 2013; Wang, Blood 2015; Gosh, JCO 2016). Although survivals seemed promising after HaploSCT, hematopoietic recovery following such a mismatched transplantation could represent a limitation. Thus, our series aims to evaluate hematological recovery after HaploSCT using a post transplantation cyclophosphamide (PT-Cy) platform.
Methods
This retrospective monocentric study included consecutive patients with following criteria: adults with hematological malignancies; bone marrow or peripheral blood T-replete HaploSCT from 2011 to 2015; non-myeloablative (Baltimore approach) or reduced intensity conditioning (busulfan-based) regimen; PT-Cy as part of GVHD prophylaxis. Patients with primary graft failure were excluded. Absolute neutrophil count (ANC), red cells (RCT) or platelet transfusion (PT) requirements on day 30 (D30) and day 100 (D100) were analyzed among disease-free patients. We first separately evaluated the rate of patients with significant cytopenia in each lineage (defined by ANC < 1 G/L, RCT need, PT need) and searched for impact of pre-transplantation factors on cytopenia (multivariate analyses by binary logistic regression). Then, we evaluated outcome by D30- and D100-landmark analyses according to cytopenia.
Results
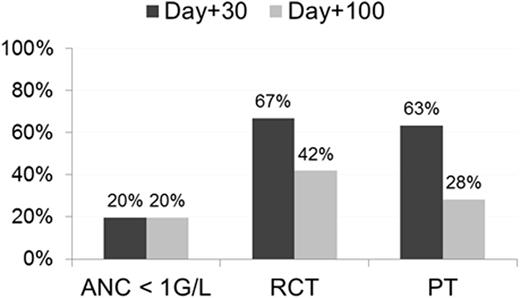
One hundred and forty six patients with a median age of 56 years (range: 19-73) were analyzed: 142 and 117 were evaluable at D30 (4 early deaths) and D100 (17 deaths, 11 relapses), respectively. At D30, 20% of patients had ANC<1G/L, 67% needed RCT and 63% needed PT. Corresponding values at D100 were 20%, 42% and 28%, respectively (Figure 1).
At D30: the use of PBSC (HR 9.5, p=0.002) was significantly associated with ANC>1G/L at D30; the use of NMAC Baltimore schema (HR 0.3, p=0.012) and CD34+ cell dose > median (HR 0.4, p=0.041) decreased PT needs while hematopoietic cell transplantation comorbidity index (HCT-CI)≥3 (HR 3.3, p=0.004) was associated with PT needs; no factor was found to significantly influence RCT.
At D100: Age>60 years (HR 2.4, p=0.045), female to male HaploSCT (HR 3.3, p=0.020) and HCT-CI≥3 (HR 3.7, p=0.006) were significantly associated with higher risk of RCT need; female to male HaploSCT (HR 3.6, p=0.015) and HCT-CI≥3 (HR 6.9, p=0.001) were associated with PT needs; no factor was found to significantly influence ANC.
With a median follow up of 25 months (range: 5-55), cox multivariate model with adjustment by age (continuous), disease risk index (low/intermediate vs high/very high), HCT-CI (0-2 vs ≥3), conditioning regimen (baltimore vs. busulfan-based) and graft source (bone marrow vs PBSC) showed that ANC<1 G/L was strongly associated with higher NRM (HR 2.9, p=0.011) and shorter OS (HR 3.4, p<0.001), overcoming the impact of RCT and PT needs (Figure 2A and 2B). In contrast, D100 analysis showed that PT need was the most determinant factor of increased NRM (HR 13.7, p=0.013) and poor OS (HR 7.3, p=0.003), while both D100 ANC and RCT needs did not impact outcome (Figure 2C and 2D).
Discussion
We found that cytopenia remain a concern after HaploSCT, leading to increased NRM and OS. The absence of ANC>1G/L at D30 as well as the need of PT at D100 may be considered as a strong post transplantation factor predicting poor outcome. Some pre-transplantation factors of cytopenia have been identified, such as CD34+ cell dose, sex mismatch and graft source. Among them, some may help for donor selection while the optimal donor for HaploSCT is still unknown. Moreover, better neutrophil recovery at D30 is achieved with the use of PBSC. CD34+ optimal cell dose in this setting remains also to be determined. In addition, post transplantation events such GVHD and/or infections should be evaluate to explore their interactions with such cytopenia, aiming to develop early therapeutic interventions.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal