Abstract
Introduction. Blood stream infections (BSIs) represent a common event during allogeneic hematopoietic stem cell transplantation (allo-SCT) and are associated with high rate of mortality. Prophylaxis with fluoroquinolones is commonly adopted to prevent severe infection during the neutropenic phase. The emerging bacterial strains resistant to these antimicrobial agents could lead to change this type of approach.
Patients and methods. We retrospectively analyzed positive blood cultures (BCs) from patients allotransplanted from January 2010 to December 2015 within our transplant program. Antimicrobial prophylaxis was conducted with a quinolone during the neutropenic period, acyclovir and fluconazole starting from the day prior to reinfusion until the withdrawn of immunosuppressive therapy and sulfametoxazole/trimethoprim starting from the hematological recovery. GVHD prophylaxis consisted on cyclosporine and methotrexate in all cases, with the addition of ATG in patients transplanted from matched unrelated donor (MUD) or with cord-blood (CB) units. Post-transplant cyclophosphamide was used in the setting of haploidentical donors. At fever onset, BCs were collected from peripheral blood (PB-BCs) and central venous catheter (CVC-BCs). A CVC related infection was defined when a positive CVC-BC proceeded by 2 hours the positivity of PB-BCs. CVC contamination was defined by the presence of positive CVC-BCs and negative PB-BCs. Empirical broad-spectrum antimicrobial therapy was usually conduct with a third or fourth generation cephalosporin with the addiction of a glycopeptide agent, if mucositis occurred.
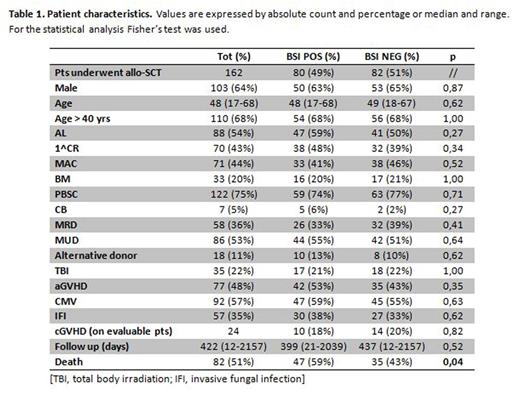
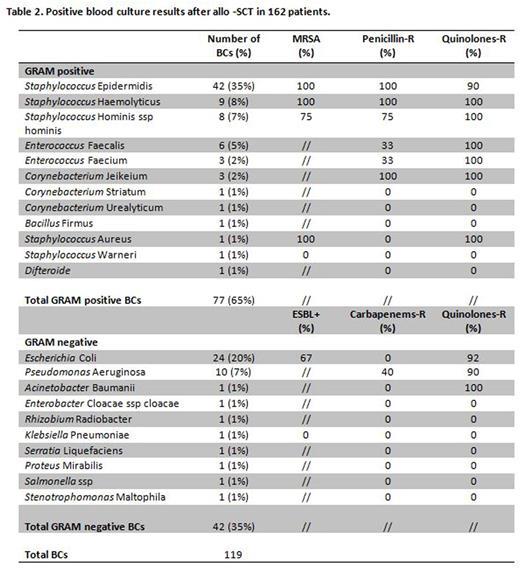
Results. One hundred-sixty-two patients underwent allo-SCT of whom 88 (54%) had acute leukemia (AL); 70 (43%) were transplanted in first CR or up-front; 71 (44%) received a myeloablative conditioning (MAC). The stem cell source was bone marrow (BM) in 33 (20%), peripheral blood stem cells (PBSC) in 122 (75%) and CB in 7 (5%) cases. Donors were matched related donor (MRD) in 58 (36%), MUD in 86 (53%) and alternative (haploidentical or CB) in 18 (11%) cases. The median time to positive BCs since allo-SCT was 13 days (range -4 - +1482). Eighty patients (49%) had a positive BCs, for a total of 119 samples. No difference in the clinical characteristics of patients with or without BSI was detected (Table 1). The median follow up was 399 days (range 21-2039) for the BSI positive group and 437 (range 12-2157) for the BSI negative (p=0.52). In 43 out of 80 patients with BSI (53%) we observed a correlation between the BCs and an organ involvement (mainly the lung in 34% of the cases). Seventy-seven (65%) and 42 (35%) out of 119 BCs were sustained by a Gram positive and a Gram negative agent, respectively. The distribution and the antimicrobial sensitivity of the different species is reported in Table 2. Briefly, S. epidermidis and E. coli were the most frequently isolated Gram positive and Gram negative bacteria, respectively (35% and 20%). 67% of E. coli were ESBL positive and 92% were resistant to fluoroquinolones. Moreover 40% and 90% of P. aeruginosa were resistant to carbapenems and to fluoroquinolones, respectively. Sixty (50%) and 59 (50%) out of 119 BCs were CVC-BCs and PB-BCs, respectively. Regarding positive CVC-BCs, 28 (24%) were CVC related BSIs; CVC contamination was observed in 21 cases (18%). The most common isolate from CVC-BCs was S. epidermidis, with 25 cases (21%). Forty -seven out of 80 patients (59%) in the BSI positive group and 35 out of 82 (43%) in the BSI negative group died (p=0.04). Overall, the infection-related mortality was 19% (15 cases). Species with the higher mortality rate were: P. aeruginosa (50%) and E. faecium (67%).
Conclusions: Prophylaxis with fluoroquinolones predominantly selects Gram positive infections the majority of which were CVC related. Infections by Gram negative strains are frequently characterized by multi-antimicrobial agent resistance. These results urge to reconsider the antimicrobial prophylaxis strategy. Prospective surveillance of BSIs is a mainstay in the management of patients addressed to allo-SCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal