Abstract
Introduction: There is an increase application of haploidentical stem cell transplantation (haplo-HSCT) based on post-transplant cyclophosphamide without T cells depletion in patients lacking identical HLA donor. One important issue in haplo-HSCT is related to immunosuppression and immune reconstitution, leading to infection complications.
Objective: To analyze the incidence and risk factors of viral infections in patients undergoing haploidentical BMT in a single Brazilian Cancer Center.
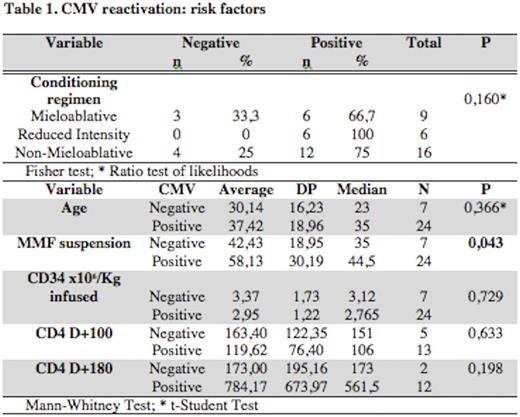
Methodology: We analyzed 31 consecutive patients with hematological malignancies (80%) and severe aplastic anemia, who underwent haplo-HSCT from 2010 to 2015. Nine patients (29%), 16 (51%), and 6 (19%) used myeloablative (MA), non-myeloablative (NMA) and reduced intensive conditioning (RIC) regimen, respectively. All grafts were T cell replete and 29 (93.5%) of the haplo-HSCT used GCSF-stimulated bone marrow source. All patients have received mycophenolate mofetil (MMF), tacrolimus, and post-transplant Cyclophosphamide (Cy) as post transplant immunosuppression. MMF was discontinued on D+35 in NMA regimen and on D+90 in MA and RIC regimen. Viral monitoring tests were performed from graft infusion to D+180 post transplant. Quantitative PCR for CMV and Adenovirus were performed weekly and quantitative PCR for EBV every 14 days. BK virus and HHV-6 quantitative PCR were performed only for patients with clinical suspicious. Besides daily absolute lymphocyte count, CD4+ T lymphocyte count was done on D+100 and D+180 post transplant. The event reactivation / viral infection was assessed in the first 6 months post haplo-HSCT.
Results: Patients median age was 34 years (range, 7 to 74). The median graft CD34+ cells infused was 2,79 x106/kg (0,56 to 5,88x106/kg), time to MMF suspension was on D+41 (range 30 to 161) and median patients engraftment was on day 18 (13 to 34). All patients achieved full donor chimerism by D+28 to 34+ post transplant. The median number of lymphocytes on D+30 and D+100, was 223x103/ul and 705x103/ul respectively, and median number of CD4+ lymphocytes on the D+100 and D+180 was 108/mm3 and 158/mm3, respectively. The cumulative incidence of viral reactivation on D+180 was 85.7%. Mortality related to viral infection was 10% and the overall survival in 180 days 74.8%. Thirty patients were CMV IgG+ (96%) and only five donors (16.1%) were CMV IgG-. First CMV reactivation occurred in 24/31 (77,4%) patients, 33,3% (8/24) had subsequent CMV reactivations. The median time of CMV reactivation was on D+41 (21-67). Documented CMV pneumonia occurred in 3 patients. Time to MMF suspension was associated to CMV reactivation (P=0,043) and we found that suspension after day + 40 had higher risk of reactivation, with sensitivity of 62,5% and specificity of 71,4% (IC 95% 0,517 - 0,989, P=0.045; ROC curve). There was no association between CMV reactivation and conditioning regimen, age, number of CD34+ cells infused (Table 1). Interestingly, age presented a linear correlation for second reactivation with an increased risk of 6% per year (HR 1.06, IC95 [1.02 to 1.11]; P=0,007). CMV reactivation was not associated with greater risk of death (P=0,194). The second more frequent viral infection was BK virus cystitis (n=11, 35.5%) and was not correlated with increased death risk (P=0,573) or any other proposed predictors factors. Parvovirus B19 infection occurred in 4 patients (12%) and adenovirus reactivation in 3 (9%). All patients who had adenovirus reactivation also had CMV reactivation and BK virus cystitis. Median lymphocytes and CD4+ counts were similarly in patients with (p = 0.385) or no (P = 0.800) CMV reactivation. The incidence of grade II-IV acute GVHD was 25.8% and there was no correlation to viral reactivation (P=0,351) or time to MMF suspension (P=0,63). However, all patients with acute GVHD II-IV showed reactivation of CMV.
Conclusion: CMV reactivations and infections in our setting seems to be higher than previously reported in the literature, probably because of high CMV IgG+ positive recipient/donor population in Brazil. Early MMF suspension (before D+40) is an effective and safe measure to control CMV reactivation in patients submitted to cy post haplo-HSCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal