Abstract
Introduction
The use of Haploidentical Transplantation (haploSCT) with pos-transplantation cyclophosphamide (PTCy) has become in a very good alternative for patients with acute leukemia who need a transplant but without a well matched donor, however, it is not clear what is the "best" conditioning regimen in this setting; on the other hand, fludarabine + melphalan (flu-mel) is a well-known preparative protocol, it has a good balance between toxicity and anti-leukemic activity. We explored the use of it plus the addition of 200-400cGy of total body irradiation (TBI) in a group of 34 patients with acute leukemia who were allografted with haplo peripheral blood stem cells (PBSC) and PTCy.
Methods and Patients
Donors were mobilized with filgrastim 5 mg/kg/BID for five days, the PBSC were collected with one or two large volume apheresis procedure. The conditioning consisted of melphalan 100-120 mgs/m2 administered on day -6, fludarabine 150 mgs/m2 split in 5 days, and 200-400 cGy of TBI added on day - 1 (Flu Mel TBI). All patients were given PTCy 50 mg/kg/day on D+3 and D+4, followed by ciclosporin and mycophenolate starting on day + 5. In all cases filgrastim was administered after transplant beginning on d + 6.
After a signed informed consent, 34 patients underwent to transplant; median age was 22 years (range 5-53), the diagnosis were: acute myeloid leukemia 11 patients, acute lymphoid leukemia 22 and 1 had myelodysplasia. 26.5% were in first remission (CR1), 47 % in second (CR2), and 26.5% in third or with more than 5% of blast in bone marrow (CR3). 5 out of 30 cases in remission had MRD positivity
Results
50% of patients received flu-mel +TBI 400 cGy, while the other half were given flu-mel + TBI 300 or 200 cGy. A mean of 12 million of PBSC/kg was infused. The neutrophil engraftment rate was 97%, median time to achieve 500 or more was 15 days (range 11-20), 3 patient died before d+ 100 without platelet recovery, the remaining had a self- sustained platelet count of 20.000 or more at an average of 15 days (range 12-48). Chimerism was available in all cases that survived beyond day + 100; all of them had full donor hematopoiesis.
The main toxicities were gastro intestinal; mucositis G II-III 35%, and two cases of hemorrhage, and bacteremia (30%). With a median follow-up for surviving patients of 11 months, the incidence of GVHD acute (GII-IV) and chronic extensive was 29.4 and 25% respectively. The transplantation related mortality was 17.4% while the rate of relapse was 14%. Causes of death were relapse: 4, sepsis: 4 fusariosis: 1, intestinal GVHD: 1.
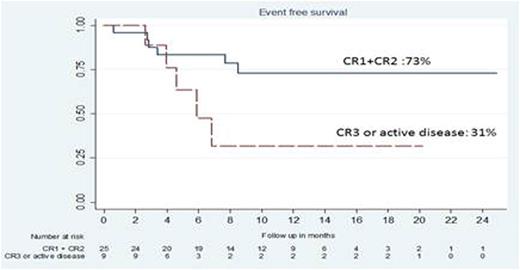
Event was defined as death for any cause or relapse, the event free survival (Kaplan Meier) at 12 and 24 months was; 63% for the whole group, 73% for CR1+CR2 and 31% for patients in CR3 or with active disease (figure 1)
Conclusion
The use of fludarabine - melphalan plus 200-400 cGy of TBI as a preparative regimen previous to transplant of haplo PBSC with PTCy was associated to a fast and almost universal engraftment, acceptable toxicity and encouraging disease free survival showing a very good balance between tolerance and anti leukemic activity. It deserve more studies
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal