Abstract
Background: Graft rejection is a significant complication following allogeneic hematopoietic cell transplantation (HCT). Heavily transfused patients with nonmalignant blood disorders, such as aplastic anemia, thalassemia major, and sickle cell anemia, had rejection probabilities in the range of 5~60% in earlier transplant series. Since rejections were seen despite the use of HLA-identical donors, rejections were attributed to sensitization to minor non-HLA antigens via transfusions. Systemic intensification of regimens with higher doses of chemotherapy or total body irradiation (TBI) lead to worse outcomes due to regimen-related mortality. In our well-established canine model, following 9.2Gy TBI conditioning, only 1.6% (1/62) of untransfused dogs rejected the marrow grafts from their dog leukocyte antigen (DLA)-identical littermate donors. However, 100% (27/27) of the dogs pretreated with three unirradiated transfusions from their respective DLA-identical marrow donors rejected their grafts. We seek to overcome graft rejection by adding monoclonal antibody (MAb)-based targeted radioimmunotherapy (RIT) with astatine-211 (211At) to conditioning with 9.2 Gy TBI. 211At is an alpha-particle-emitting isotope, which has a short path length (0.06 mm), very high energy, and high cytotoxicity of alpha emissions. These properties and the short half-life (7.2 hours) may reduce early toxicities as well as late effects, such as secondary malignancies. The purpose of this study is to determine the quantity of 211At required to provide durable donor engraftment in DLA-identical HCT when 211At-labeled anti-CD45 MAb is used in combination with TBI to condition transfusion-sensitized dogs.
Methods: Five recipients were given three preceding transfusions of 50 mL unirradiated whole blood from their respective DLA-identical marrow donors on days -24, -17, and -10, followed by 211At-labeled anti-CD45 MAb on day -3 and 9.2 Gy TBI and a marrow transplant on day 0. The injected 211At activity ranged between 0.188 and 0.304 mCi/kg body weight labeled on 0.5 mg/kg anti-CD45 MAb. Ten percent of the total dose of anti-CD45 MAb was administered as unlabeled MAb prior to infusion of the radiolabeled MAb in order to prevent nonspecific tissue binding of the radiolabeled MAb. Dogs received marrow containing a mean of 5.1 x 108 (range, 1.3-8.3) total nucleated cells/kg and 2.8 x 106 (range, 0.4-5.5) CD34+cells/kg. Dogs did not receive post-grafting immunosuppression.
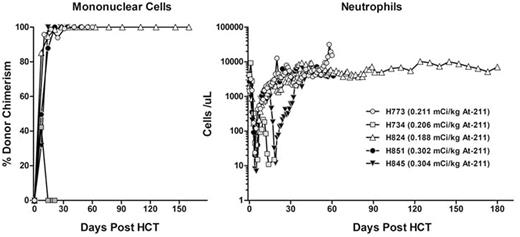
Results: Results are shown in Figure 1. Granulocyte nadirs (median, 20/µL) and platelet nadirs (median, 4500/µL) occurred at a median time of 5 days and 11 days, respectively. Neutrophil engraftment (>=500/µL, 3 consecutive days) and platelet engraftment (>=20,000/µL, 7 consecutive days, without transfusion) were achieved at a median of 8 (7-9) days and 20 (18-21) days, respectively. Four dogs achieved 100% donor chimerism in mononuclear cells, granulocytes, and CD3+ T-cells. Only one dog rejected the graft on day 14 after transplantation. That dog received the lowest numbers of CD34+ and marrow cell dose (0.35 x 106 CD34+ and 1.3 x 108 total nucleated cells per kg, respectively), which could be one of the reasons for the graft rejection. After a median follow-up time of 60 (21-182) days, no renal toxicity had been observed. One dog was euthanized on day 60 due to liver toxicity (CTCAE grade 4), but there was no evidence of GVHD on histopathological evaluation.
Conclusions: The preliminary results are encouraging and show that 211At-labeled anti-CD45 MAb in combination with TBI as conditioning is successful in establishing sustained DLA-identical grafts in 4/5 dogs, especially when compared to previous studies showing that 100% of the dogs (27/27) rejected their grafts when pretreated with three unirradiated transfusions from their marrow donors. We will increase the sample size and then proceed to study canine models of human blood disorders to further determine the optimal dosing of 211At in disease settings. In view of the potential of RIT, 211At-anti-CD45 RIT in conjunction with TBI may serve as a novel promising strategy to overcome graft rejection.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal