Abstract
Introduction
Maintenance therapy after first-line ASCT improves outcomes, although virtually all pts eventually relapse. The pattern of first relapse shows significant heterogeneity. The literature is scarce about the impact of maintenance on the pattern of relapse and about predictors of a more aggressive or indolent relapse course. Our objectives were, in a cohort of transplant-eligible MM pts treated with a CyBorD induction regimen followed by ASCT as part of first-line therapy, to describe the pattern of first relapse, to determine if patterns differ between pts with and without maintenance and to identify predictors for patterns of first relapse, early relapse, PFS, OS and OS after relapse in the real-world setting.
Methods
Inclusion criteria were MM pts who received at least 2 cycles of induction with a CyBorD regimen with their induction regimen start date from January 2007 to December 2012. Pts then underwent single (126) or tandem ASCT (10) in first-line. Primary refractory disease was excluded. Charts were retrospectively reviewed for descriptive and univariate analysis. The pattern of relapse was categorized as biochemical, clinical, clinical with extramedullary disease or clinical with plasma cell leukemia.
Results
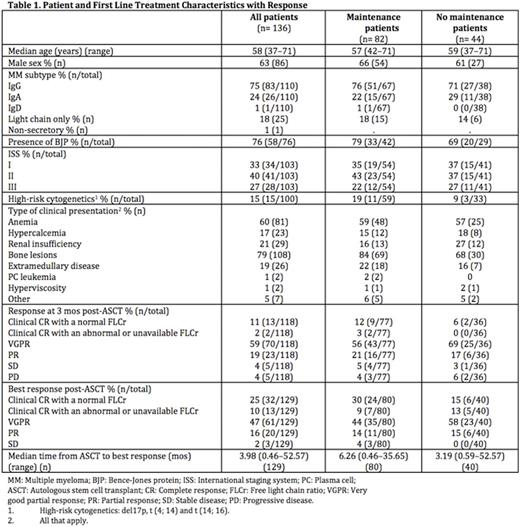
Median follow-up of the 136 pts was 43.4 months (mos). Pt and first-line treatment characteristics are presented in Table 1. Most pts presented with anemia and bone lesions. The maintenance (n= 82; lenalidomide= 84%, thalidomide= 13%, lenalidomide and bortezomib= 2%) and no maintenance (n= 44) groups were similar, except for fewer pts with high-risk cytogenetics in the no maintenance group (9% vs 19%). All 10 tandem ASCT pts had maintenance. Response rates at 3 mos post-ASCT and best response rates after ASCT were similar between the maintenance and no maintenance groups (VGPR or better response rates were respectively 70% and 83% for the maintenance group and 75% and 85% for the no maintenance group) (Table 1). The median duration of maintenance was 11.1 mos (0.5-55.1) and 56% had stopped for progression.
Overall median PFS was 41.3 mos (95%CI= 34.6-54.3) and overall median OS was 96.7 mos (95%CI lower bound= 64.9). For pts on lenalidomide maintenance, median PFS was 51.5 mos (95%CI= 35.9-61.8) and median OS was not reached on the study duration. Pts on maintenance had a significantly shorter median OS after relapse when compared to pts without maintenance (9.2 vs 19.9 mos, p= 0.006).
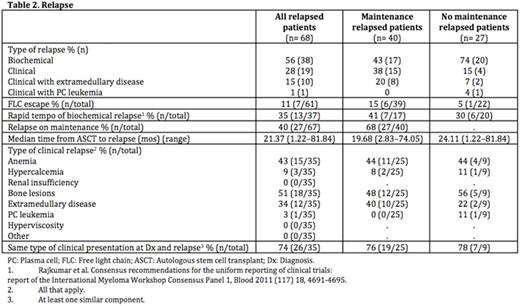
Sixty-eight pts relapsed (50%), 40 in the maintenance group and 27 in the no maintenance group (Table 2). Overall, biochemical relapse was the most frequent type of relapse (56%) in all pts. However, pts receiving maintenance more often relapsed clinically and pts in the no maintenance group more often experienced biochemical relapses. Six of the 7 cases of FLC escape (86%) were in the maintenance group. Clinical relapsers usually had at least 1 component of the clinical presentation at relapse that was the same as at diagnosis (Dx). Overall, the most frequent types of clinical relapse involved bone lesions (51%), anemia (43%) and extramedullary disease (34%), the latter being more frequent in the maintenance group (40% vs 22%).Correlations between hypercalcemia at Dx and at relapse (positive correlation; coefficient= 0.45, p= 0.0064) and extramedullary disease at Dx and at relapse (positive correlation; coefficient= 0.39, p= 0.0201) were significant.
By univariate analysis, maintenance (OR= 3.866, 95%CI= 1.333-11.211, p= 0.013) and high LDH at Dx (OR= 1.009, 95%CI= 1.001-1.016, p= 0.027) were associated with a clinical pattern of relapse. Bone lesions versus no bone lesions at progression were: 1) less likely to relapse early (OR= 0.178, 95%CI= 0.037-0.849, p= 0.030); 2) had a significantly longer median PFS (34.3 vs 15.6 mos, p= 0.0002); 3) had a longer OS (79.4 vs 36.3 mos, p= 0.031) and 4) had a longer OS after relapse (13.9 vs 3.7 mos, p= 0.003).
Conclusions
The most common pattern of first relapse was biochemical. Although we cannot exclude an effect of pt bias regarding use of maintenance, we observed an impact of maintenance on the pattern of relapse, with more clinical relapses. For pts relapsing on maintenance, cases of FLC escape and of extramedullary disease at relapse were also more frequent and OS after relapse tended to be shorter. High LDH at Dx was also associated with a clinical pattern of relapse. Interestingly, pts presenting with bone lesions at progression had better outcomes.
Cote:Takeda: Honoraria; Janssen: Honoraria. Reece:Celgene: Consultancy, Honoraria, Research Funding; Janssen: Consultancy, Honoraria, Research Funding; Takeda: Consultancy, Honoraria, Research Funding; BMS: Honoraria, Research Funding; Amgen: Consultancy, Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Merck: Research Funding; Otsuka: Honoraria, Research Funding. Chen:Takeda: Research Funding; Janssen: Honoraria, Research Funding; Celgene: Honoraria, Research Funding. Prica:Celgene: Honoraria; Janssen: Honoraria. Tiedemann:Janssen: Honoraria; Celgene: Honoraria. Trudel:Amgen: Honoraria; Oncoethix: Research Funding; BMS: Honoraria; Glaxo Smith Kline: Honoraria, Research Funding; Novartis: Consultancy, Honoraria; Celgene: Consultancy, Equity Ownership, Honoraria. Kukreti:Lundbeck: Honoraria; Celgene: Honoraria; Amgen: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal