Abstract
Background:Monitoring of serum free light chain (sFLC) ratio after treatment in multiple myeloma (MM) patients is valuable for assessing monoclonal component of free light chain (FLC). However, the recent International Myeloma Working Group guidelines did not recommend replacing 24-hour urine analysis with FLC analysis in diagnosis or response assessment of MM, and previous studies indicated discordance between urine analysis and sFLC levels in light chain-only MM (LCMM). This is clinically relevant because sFLC normalization was considered a surrogate for improved outcome in both LCMM and intact immunoglobulin MM (IIMM). The clinical impact of FLC ratio normalization on detection of monoclonal component may differ between LCMM or oligosecretory myeloma (OSMM) and IIMM. This study explored the utility of sFLC ratio as a surrogate for residual clonal monoclonal component compared with 24-hour urine immunofixation electrophoresis (uIFx) after treatment. We evaluated the impact of normalization of sFLC ratio in patients with LCMM/OSMM that obtained very good partial response (VGPR), complete response (CR), and immunophenotypic CR (iCR; sIFx/uIF negative plus ≤ 10-4 clonal PCs) determined by multicolor flow cytometry (MFC).
Methods:We included 176 patients (51 with LCMM and OSMM, 125 with IIMM) treated between April 2006 and January 2016 at Kameda Medical Center, Japan. Immunoglobulin levels in serum and urine samples were examined by serum protein electrophoresis (SPEP), serum immunofixation electrophoresis (sIFx), urine protein electrophoresis (UPEP), uIFx, and sFLC for response assessment. Minimal residual disease (MRD) assessments after treatment were performed by 6-color MFC and the results were compared to other tests of monoclonal components, including SPEP, UPEP, sIFx, uIFx, and FLC. Agreement between sFLC normalization and MRD by MFC was assessed using kappa statistic. Disease response was evaluated using IMWG criteria. sFLC was measured by Fleelite® assay (The Binding Site Group Ltd.). Reference ranges for sFLC have been previously published. Statistical analyses were performed with EZR, which is a graphical user interface for R ver. 3.2.1.
Ethical considerations:This study was approved by the local ethics committee and conducted in accordance with the Declaration of Helsinki and Good Clinical Practice Guidelines.
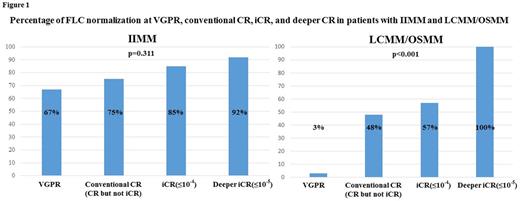
Results: All of 51 LCMM/OSMM patients (100%) and 95 of the 125 IIMM patients (72%) had measurable and abnormal involved sFLC (≥ 100 mg/L) and positive uIFx at presentation. VGPR, CR, and iCR were obtained in 31 (61%), 25 (49%), and 14 (27%) patients with LCMM/OSMM, respectively, and normalization of sFLC ratio at VGPR, CR and iCR was seen in 1/31 (3%), 13/25 (48%), and 8/14 (57%) of these patients, respectively. Among the LCMM/OSMM patients with iCR, 4 patients obtained deeper iCR (≤ 10-5 clonal PCs) and all of them had normal sFLC ratio, while sFLC ratio remained abnormal in the rest of 10 iCR patients that did not achieve deeper iCR. In IIMM patients, VGPR, CR, and iCR were obtained in 78 (61%), 52 (42%), and 20 (16%) patients, respectively. In contrast to the LCMM/OSMM patients, normalization of the sFLC ratio at VGPR, CR, and iCR was seen in 52/78 (67%), 39/52 (75%), and 17/20 (85%) of IIMM patients, respectively. Thirteen of the 14 IIMM patients (93%) that obtained deeper iCR had normal sFLC ratio. Among the patients with IIMM, percentage of patients with normalized sFLC ratio did not differ between the response groups (p=0.11), while it was significantly different in LCMM/OSMM patients (p<0.001) (Figure 1). These observations indicated that the normalization of sFLC ratio is significantly associated with deeper response in LCMM/OSMM patients, but not in IIMM patients.
Conclusions:Our observations indicated that sFLC test has greater sensitivity than urine immunofixation for detection of the monoclonal component of sFLC, especially in patients with LCMM/OSMM. In addition, we also showed that normalization of sFLC ratio is correlated with the depth of response assessed by MFC in patients with LCMM/OSMM, but not in IIMM patients. These findings suggest that FLC ratio provides greater sensitivity for residual disease monitoring than uPEP or uIFx in patients with LCMM and OSMM, and therefore could be considered as an alternative to urine analysis for monitoring of LCMM/OSMM patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal