Abstract
Background: To investigate the impact of additional chromosomal abnormalities(ACA) in Philadelphia-positive clone on response to TKIs and long-term survival of CML patients treated with tyrosine kinase inhibitors (TKIs) in the real world.
Methods:In this retrospective study, patients with chronic myelogenous leukemia (CML) in chronic phase treated with TKIs were recruited. The chromosome banding analysis was performed on bone marrow cells at baseline and during the TKIs therapy.The clinic response to TKIs was evaluated according to the recommendation of ELN2013. The overall survival (OS), events free survival (EFS) and progression free survival (PFS) were analyzed. Events were defined as treatment failure, progression to accelerate phase or blast crisis and death. The progression was defined according to criteria of ELN2013 CML recommendation.
Results:
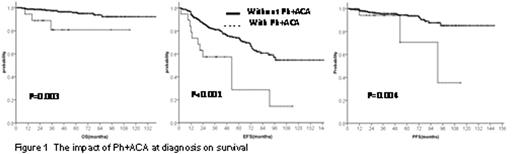
The characters and cytogenetic analysis of the patients:A total of 451 patients (281 males and 170 females) were enrolled from Jun 2004 to March 2015.The median age was 42 (range 18-79) years old. 414 subjects hadevaluable information of karyotypeat baseline.351 patients (84.4%) had the standard Philadelphia chromosome (Ph), 8(1.9%) showed variant translocation of Ph, 19 had ACA in Ph+ cells (Ph+ACA), only 2(0.5%) showed ACA in Ph- cells (Ph-ACA)£¬11(2.7%) had normal karyotype. 29 patients (6.4%) developed Ph+ACA during the TKIs treatment. Ph-ACA occurred in 8 subjects (6.4%).The response to TKIs: Comparing to the patients without Ph+ACA at baseline, the patients with Ph+ACA had lower cumulative rate of complete cytogenetic response (CCyR) (92.4% vs 68.4%, P=0.038) and prolonger median time to achieving CCyR (19 vs 7 months, P=0.016).The Ph+ACA at diagnosis had no effect on achieving major molecular response (MMR). The OS, EFS and PFS at 7 years for the whole cohort were 91%¡¢54% and 83% respectively. The patients with baseline Ph+ACA had significant inferior survival comparing to the subjects without Ph+ACA (Figure 1). The median time of OS, EFS, PFS for Ph+ACA patients were 108, 50 and 91 months, whereas the patients without Ph+ACA were not reached ( P=0.003 for OS, P<0.001 for EFS, and P=0.004 for PFS). The patients developed Ph+ACA during treatment had similar OS comparing to the subjects with Ph-ACA or without ACA (P=0.115), but they had significant shorter EFS (31 vs 90 months vs not reached£¬P<0.001)and PFS(59 vs 120 months vs not reached£¬P<0.001).
Conclusion: The Ph+ACA emergence at diagnosis and during treatment had negative impact on prognosis of CML patients treated with TKIs.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal