Abstract

Background:
Discontinuation of tyrosine kinase inhibitor (TKI) treatment for chronic myeloid leukaemia (CML) patients in stable deep molecular response leads to treatment-free remission (TFR) in approximately 50% of cases. In most studies, monthly PCRs was performed for 12 months followed by 2-3 monthly testing thereafter. Around 80% of molecular relapses occur within the first 6 months after TKI cessation. The current recommendation for TKI recommencement is a single BCR-ABL1 value ≥0.1% IS (International scale), indicating loss of major molecular response (MMR).
Not all institutions can offer monthly PCR monitoring due to financial constraints, particularly relevant in developing countries. For some patients, remaining on TKI is a cheaper alternative.
Aim:
To assess the safety of less frequent BCR-ABL1 monitoring for detection of loss of MMR for CML patients attempting TFR.
Methods:
We monitored 85 patients who ceased TKI with the aim of achieving TFR. Patients had a minimum of 24 months of sustained MR4 (n=3) or MR4.5 (n=82) prior to TKI cessation. At the time of TKI cessation, 64 patients were on imatinib (75%), 17 on nilotinib (20%) and 4 on dasatinib (5%). Forty of the patients were enrolled in the TWISTER study where the criteria for TKI recommencement was loss of MMR or 2 consecutively rising BCR-ABL1 positive values. The remaining patients were on a registry study and the trigger for TKI recommencement was loss of MMR.
Results:
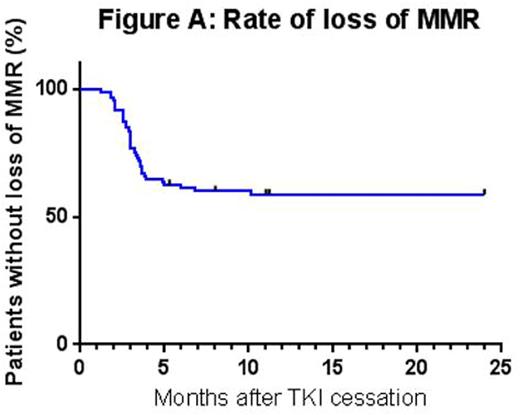
TKI recommencement occurred in 49 of 85 patients. Median time to TKI recommencement was 4 months (range 2-28 months) at a median BCR-ABL1 value of 0.27% on the International Scale (IS), range 0.002-24% IS. Thirty-six of the 49 patients (73%) lost MMR prior to TKI recommencement; the median time to loss of MMR was 3 months (range 1 to 10 months). One patient lost MMR within the first month. Figure A demonstrates the time to loss of MMR in the 36 patients with PCR values ≥ 0.1%. Eighteen of the 36 patients (50%) lost MMR by the 3 month BCR-ABL1 assessment and 35 of 36 patients (97%) lost MMR by 6 months. The latest loss of MMR was at 10 months. Fourteen patients recommenced TKI at a BCR-ABL1 value of >1% and 1 recommenced at a value >10%. Clinician delay in TKI recommencement of 1 month resulted in a BCR-ABL1 rise from 0.84% to 24% with associated loss of complete hematological response.
We propose monthly BCR-ABL1 testing between 2 and 6 months post TKI cessation followed by 2 monthly testing. Detection of a BCR-ABL1 value of ≥0.1% would trigger TKI recommencement. In the presence of a rising BCR-ABL1, which remains ≤0.1%, monthly monitoring should ensue in order to avoid hematological relapse. If this strategy were employed in this cohort of patients, only 1 patient would have had the trigger for TKI recommencement delayed by 1 month (estimated BCR-ABL1 at recommencement ~2.5%). This patient had loss of MMR in the first month post TKI cessation. If this molecular monitoring strategy was applied to patients in our cohort who had not lost MMR at TKI recommencement, we estimate that 1 other patient would have had TKI recommencement delayed by 1 month based on the average BCR-ABL1 doubling time of 1 log per month.
A proportion of patients maintain low levels of BCR-ABL1 after TKI cessation and do not lose MMR. There were 2 such patients in our cohort.
Conclusion:
The critical time for molecular monitoring to trigger TKI recommencement is the first 6 months. A monthly monitoring strategy beginning 2 months after cessation would capture the majority of patients at loss of MMR. The data suggest that after 6 months, 2-monthly monitoring could follow. Monthly BCR-ABL1 testing can be re-introduced in the event of a positive result in those that ceased TKI with undetectable BCR-ABL1 or if there is a BCR-ABL1 result higher than the cessation value. This approach would reduce BCR-ABL1 testing by approximately 33% in the majority of cases while minimizing hematological relapse. Therefore this strategy would reduce the cost and inconvenience of molecular monitoring for a trial of TKI cessation, making the option of TFR available to some patients for whom it is otherwise not feasible.
Branford:Qiagen: Honoraria, Membership on an entity's Board of Directors or advisory committees; Cepheid: Consultancy; Ariad: Research Funding; Bristol Myers Squibb: Research Funding; Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding. Yeung:BMS: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis Pharmaceuticals: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Ariad: Research Funding. Ross:Novartis Pharmaceuticals: Honoraria, Research Funding; BMS: Honoraria. Hughes:Bristol-Myers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Ariad: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis Pharmaceuticals: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Australasian Leukaemia and Lymphoma Group (ALLG): Other: Chair of the CML/MPN Disease Group.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal