Abstract
Background
It has been well known that peripheral T cell lymphoma (PTCL) has undergone poor prognosis compared with other non-Hodgkin lymphomas (NHL). Although the National Comprehensive Cancer Network-International Prognostic Index (NCCN-IPI) has been proposed to determining prognosis for patients with diffuse large B-cell lymphoma (DLBCL) at 2014, there is no study examines whether NCCN-IPI could apply to the T-cell NHLs. In addition, a few studies suggest prognostic utility of interim PET/CT in PTCL, but the role of interim PET/CT is not clear.
Purpose
We evaluate the predictive efficacy of the NCCN-IPI and interim PET/CT based on visual assessment in patients with newly diagnosed PTCLs.
Methods
This study included 153 patients with de novo peripheral PTCLs, diagnosed from January 2010 to August 2015. The NCCN-IPI was calculated as following the original references. Survival outcomes were compared with a matched result of IPI and/or Prognostic Index for peripheral T cell lymphoma, unspecified (PIT). Visual assessment of interim PET/CT based on Deauville five point scales was performed at the time of diagnosis, mid-treatment and completion of CHOP/CHOP-like or other non-anthracycline chemotherapy.
Results
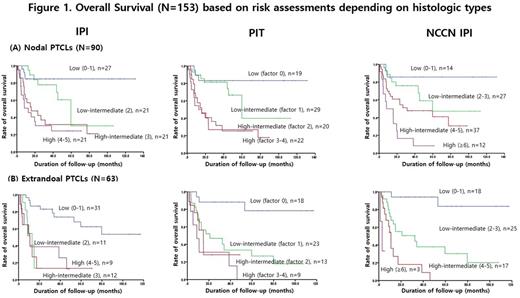
The subtypes of PTCLs included PTCL, not otherwise specified (PTCL-NOS) (26%), angioimmunoblastic T cell lymphoma (20%), anaplastic large cell lymphoma (13%), extranodal NK/T cell lymphoma, nasal type (35%), and the others (6%). The NCCN-IPI showed better risk-based prognostic discrimination than IPI and PIT, especially between high-intermediate and high risk subgroups (3-year overall survival 40% vs. 27% vs. 26% among the high-intermediate risk group, respectively; 3-year overall survival 15% vs. 33% vs. 32% among the high risk group, respectively) with a median follow-up of 25.1 months (Figure 1). The absolute difference of survival rates between the low and high risk groups was 75% based on the NCCN-IPI stratification compared with 45% on the IPI stratification or 54% on the PIT stratification, respectively. When divided into two histologic subgroups (nodal vs. extra-nodal type), the NCCN-IPI showed considerable discriminatory capacity in both histologic groups. However, the IPI or PIT classification could not have discrimination in extra-nodal PTCLs. The interim PET-CT was significantly predicting for progression free survival in all PTCL patients, however, it also showed no predictive value in the patients with extranodal PTCLs, especially NK/T cell lymphoma.
Conclusions
The NCCN-IPI is a powerful prognostic model in PTCLs predicting overall survival among high-intermediate and high risk patients. Also, interim PET/CT response based on visual assessment could be a valuable prediction tool in nodal PTCLs, however, it should be carefully interpreted in the treatment of extranodal subtypes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal