Abstract
Introduction: "High grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements" (HG DH/THL) is a new diagnosis per the revised 2016 WHO classification. It has been colloquially called "double hit/triple hit lymphoma" and is significant for its aggressive clinical course. However, under this umbrella diagnosis there are several morphologic and cytogenetic variants with either controversial or unknown clinical significance. Herein, we investigate the prognostic significance of several of these parameters, including morphology, immunoglobulin gene (IG) vs non-IG MYC translocation partners, and BCL2/BCL6 translocation status in HG DH/THL in the Mayo Clinic Rochester practice.
Materials and methods: All cases, which were identified through the Mayo Clinic Lymphoma Database, University of Iowa/Mayo Clinic SPORE Molecular Epidemiology Resource (MER), and the Mayo Clinic Cytogenetics Laboratory, had diffuse large B-cell lymphoma (DLBCL) or high grade B-cell lymphoma (HGBCL) morphology, were CD20-positive, and had a MYC translocation with concurrent BCL2 and/or BCL6 translocations. Morphology was re-reviewed by four hematopathologists when possible. Cell of origin (germinal center B-cell (GCB) vs non-GCB phenotype) was determined by paraffin section immunohistochemistry using the Hans classifier. Interphase FISH was performed on either tissue paraffin sections or bone marrow aspirate smears using a breakapart probe for MYC, followed by dual fusion probes for IGH/MYC, IGL/ MYC and IGK/MYC, a BCL6 breakapart probe, and either a BCL2 breakapart probe or an IGH/BCL2 dual fusion probe. Outcome analysis was restricted to patients with de-novo HG DH/THL or HG DH/THL at transformation of a previously diagnosed low-grade lymphoma and who were treated with anthracycline-based chemotherapy. Overall survival (OS) was defined as time from DH/THL diagnosis to death from any cause.
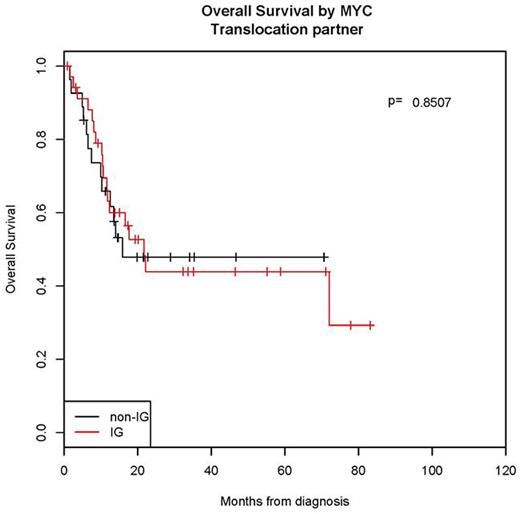
Results: There were 100 patients with a median age of 61 years (range 29-87). The consensus re-review morphologic diagnosis (n=65) was HGBCL in 39 (60%) and DLBCL in 26 (40%). The HGBCL group had inferior survival (2-year OS = 35%) compared to DLBCL (2-year OS=62%, p= 0.058). By interphase FISH, the MYC translocation partner was an IG gene (IG/MYC) in 52 cases (60%; 39 IGH, 6 IGK and 7 IGL) and a non-IG gene (non-IG/MYC) in 35 cases (40%). No difference in OS was identified between IG/MYC and non-IG/MYC cases (p=0.85, Figure 1). By FISH, 87 cases (87%) had a BCL2 translocation (59 MYC/BCL2, 20 MYC/BCL2/BCL6, and 8 MYC/BCL2/[BCL6 unknown]) and 13 (13%) lacked a BCL2 translocation (MYC/BCL6). Those with a BCL2 translocation were all of GCB phenotype (N=85), while 6 of 12 of the MYC/BCL6 cases (50%) were of non-GCB phenotype (p <0.0001). All 13 MYC/BCL6 cases were de novo diagnoses, while 38% of cases with a BCL2 translocation represented either transformation (n=22) or recurrence (n=11) events (p=0.025). The MYC/BCL6 group had better survival (2-year OS=73%) than those with BCL2 translocation (2-year OS=43%, p= 0.13).
Conclusion: As HG DH/THL's frequently have morphologic characteristics of DLBCL (40% in this series), it is important to perform complete interphase FISH analysis on all cases with DLBCL or HGBCL morphology to exclude the possibility of HG DH/THL. Furthermore, within the diagnosis of HG DH/THL, there are several morphologic and cytogenetic subtypes that are biologically and clinically significant. High grade morphology (HGBCL) tends to predict for a more aggressive clinical course independent of all other parameters (p= 0.058). Unlike a recent report (Blood 2015;126:2466), our data suggest MYC translocation partner (IG versus non-IG) may have no impact on overall survival (Figure 1). HG DH/THL's with a BCL2 translocation appear restricted to GCB phenotype, frequently represent either transformation or recurrence events, and tend to have inferior OS. In contrast, those without BCL2 translocations may be of either GCB or non-GCB phenotype, typically arise de novo, and tend to have a superior OS. Careful morphologic review and complete interphase FISH studies are essential in all HG DH/THL for prognostic and potential therapeutic purposes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal