Abstract
Background: B-cell lymphomas with a MYC/8q24 rearrangement coupled with translocations involving BCL2 and/or BCL6, often referred to as double hit or triple hit (DH/TH) lymphomas, typically have an aggressive clinical course. A new WHO subtype, "high grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements", has been established for this entity (Swerdlow et al. Blood; 127: 2375-2390, 2016). Herein we report the treatment and outcomes of DH/TH patients at our institution.
Materials and Methods: Cases were identified through the Mayo Clinic Lymphoma Database, University of Iowa/Mayo Clinic SPORE Molecular Epidemiology Resource (MER), and the Mayo Clinic Cytogenetics Laboratory. Interphase FISH was performed clinically on either paraffin sections of the tissue specimens or on smears of the bone marrow aspirate specimens using break-apart probes for MYC and BCL6, dual fusion probes for IGH/MYC, IGL/MYC, and IGK/MYC, and either a BCL2 break-apart probe or an IGH/BCL2 dual fusion probe. Consensus pathology re-review was performed to define morphology as diffuse large B-cell lymphoma (DLBCL) vs. high-grade B-cell lymphoma (HGBCL). Patients with de-novo DH/TH or diagnosis of DH/TH at the time of transformation of a previously diagnosed low-grade lymphoma and who were treated with anthracycline-based chemotherapy were included in this analysis. Patients with DH/TH first identified at the time of recurrent aggressive B-cell lymphoma were excluded. Overall survival (OS) was defined as time from DH/TH diagnosis to death from any cause. EFS12 was defined as event-free status 12 months from diagnosis of DH/TH.
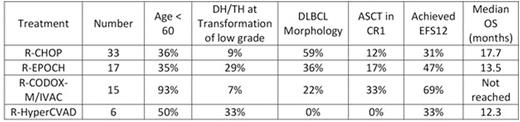
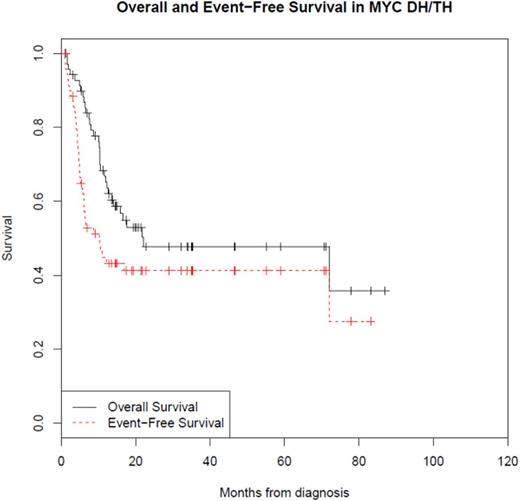
Results: Clinical outcome analysis was performed on 71 patients (Table 1). The median age was 61 years (range 29-82). 60 patients had de-novo DH/TH and 11 patients had transformation of a previously diagnosed low-grade lymphoma. In 65 cases in which there was consensus morphology on pathology re-review, there were 39 (60%) with HGBCL morphology and 26 (40%) with DLBCL morphology. At a median follow-up of 21 months (range 1-87), the event free survival at 12 months was 43%, and the median overall survival (OS) was 22 months (95% CI: 13-NA). The OS at 5 years was 48% (95% CI: 36%-63%). Patients with DH/TH at transformation of previously diagnosed low-grade lymphoma had a very poor outcome (median OS=10.8 months, EFS12 = 10%), which was inferior to patients with de-novo DH/TH (P=0.0069). When compared to all other therapies, patients treated with R-CODOX-M/IVAC had better EFS12 (p=0.03) with a trend in improved OS (p=0.08) though this may be confounded by patient selection bias as these patients were significantly younger (p=0.0001) than patients treated with other anthracycline based regimens (table 1).
Conclusion: In "high-grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements", induction failure occurs early. Although transformation to DH/TH from previously diagnosed low-grade lymphoma is associated with a particularly poor outcome, the overall survival for the entire cohort at 5 years was 48%, suggesting long-term cures in a subset of patients. Treatment with R-CODOX-M/IVAC may result in superior outcomes in patients less than 60 years of age.
Ansell:BMS, Seattle Genetics, Merck, Celldex and Affimed: Research Funding. Nowakowski:Celgene: Research Funding; Morphosys: Research Funding; Bayer: Consultancy, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal