Abstract

Background: The American College of Chest Physicians (ACCP) guidelines for venous thromboembolism (VTE) disease recommend treatment with anticoagulation for at least 3 months in patients with VTE. Moreover, the EINSTEIN-extension study assessed the effect of rivaroxaban on the risk of VTE recurrences in patients who had completed 6 to 12 months of treatment for VTE. Results showed that rivaroxaban significantly reduced the risk of VTE recurrences with a small increased risk of major bleeding. The objective of this study was to assess the risk of VTE recurrences and major bleeding associated with extended rivaroxaban treatment in a real-world setting among all VTE patients (i.e., unprovoked, provoked, and cancer related).
Methods: A retrospective study was conducted using Truven Health Analytics MarketScan Databases from 02/2011 to 04/2015. The study included adult patients who initiated rivaroxaban therapy within 7 days after their first VTE and continuously used rivaroxaban for at least 3 months. The end of the initial 3-month rivaroxaban treatment was defined as the index date and patients were categorized into discontinued (treatment ended) and continued cohorts. Patients were followed from index date until end of continuous treatment for the continued cohort or end of data or re-initiation of oral anticoagulant therapy for the discontinued cohort. The outcomes included VTE recurrences identified as a primary diagnosis documented during a hospitalization and major bleeding events identified by a validated algorithm (Cunningham et al., 2011). Kaplan-Meier rates for VTE recurrences and major bleeding events at 3, 6, 9, and 12 months after the index date were compared between cohorts with adjustment for baseline confounding using the inverse probability of treatment weights (IPTW) method based on propensity score. Patients with unprovoked VTEs, defined as not having recent surgery, cancer, pregnancy or estrogen therapy, were also evaluated. Sample sizes of patients with provoked VTEs and cancer were too small to analyze these populations. A sensitivity analysis was also conducted among VTE patients receiving rivaroxaban for at least 6 months.
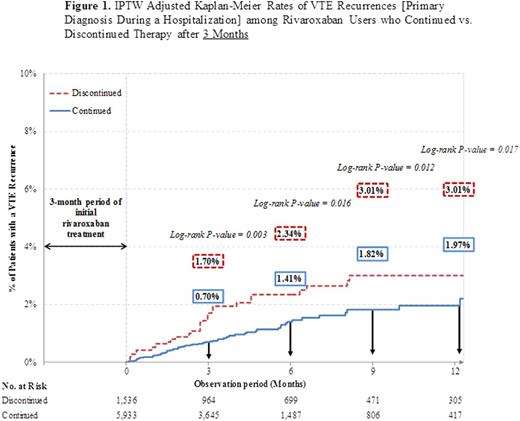
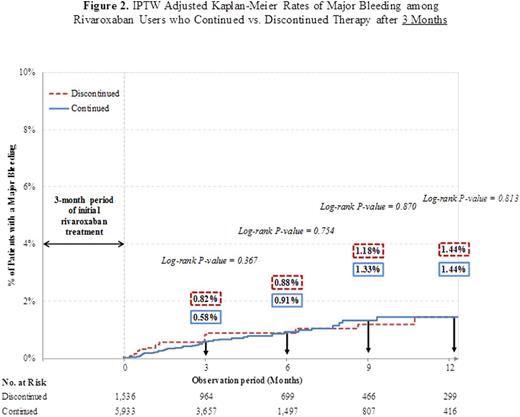
Results: Among the 3-month treatment population, a total of 5,933 (63.4% unprovoked VTE) and 1,536 (68.4% unprovoked VTE) rivaroxaban users formed the continued and discontinued cohorts, respectively. The mean (SD) observation period was 149.3 (124.4) days in the continued cohort and 211.1 (191.6) days in the discontinued cohort. The Kaplan-Meier analysis (Figure 1) showed that patients in the continued cohort had significantly lower rates of VTE recurrences after an additional 3 months (0.70% vs. 1.70%), 6 months (1.41% vs. 2.34%), 9 months (1.82% vs. 3.01%), and 12 months (1.97% vs. 3.01%; all p-values < 0.05) of treatment. No statistically significant differences in the cumulative event rates for major bleeding (Figure 2) were observed between the continued and the discontinued cohort at 3 months (0.58% vs. 0.82%), 6 months (0.91% vs. 0.88%), 9 months (1.33% vs. 1.18%), and 12 months (1.44% vs. 1.44%; all p-values > 0.05).
Among the 6-month treatment population, a total of 2,676 (65.9% unprovoked VTE) and 1,127 (70.4% unprovoked VTE) rivaroxaban users formed the continued and discontinued cohorts, respectively. The mean (SD) observation period was 158.5 (130.6) days in the continued cohort and 206.5 (171.5) days in the discontinued cohort. Patients in the continued cohort had lower rates of VTE recurrences after an additional 3 months (0.82% vs. 1.41%), 6 months (1.22% vs. 2.69%), 9 months (1.35% vs. 3.02%), and 12 months (1.72% vs. 3.70%; except at 3 months all p-values < 0.05) of treatment. No differences in the cumulative event rates for major bleeding were observed between the continued and the discontinued cohorts.
Similar results were found among patients with unprovoked VTE for the 3- and 6-month analyses. The interaction term between the cohort variable (Continued vs. Discontinued) and the type of VTE (unprovoked vs. other types of VTE) was non-significant in both populations (p-value > 0.05), which suggests that the benefit of extended treatment do not depend on the type of VTE events.
Conclusions: Our study results suggest that all patients with VTE who continued rivaroxaban therapy after the first 3-month and 6-month treatment periods had significantly lower risk of VTE recurrences without an increased risk of major bleeding.
Khorana:Halozyme: Consultancy, Honoraria; Sanofi: Consultancy, Honoraria; Pfizer: Consultancy, Honoraria; Bayer: Consultancy, Honoraria; Amgen: Consultancy, Honoraria, Research Funding; Leo: Consultancy, Honoraria, Research Funding; Roche: Consultancy, Honoraria; Janssen Scientific Affairs, LLC: Consultancy, Honoraria, Research Funding. Berger:AZ: Research Funding; Merck: Membership on an entity's Board of Directors or advisory committees. Wells:BMS/Pfizer: Research Funding; Itreas: Other: Served on a Writing Committee; Janssen Pharmaceuticals: Consultancy; Bayer Healthcare: Other: Speaker Fees and Advisory Board. Seheult:Janssen Scientific Affairs, LLC: Consultancy. Ashton:Janssen Scientific Affairs, LLC, Raritan, New Jersey: Employment. Laliberté:Janssen Scientific Affairs: Research Funding. Crivera:Janssen Scientific Affairs, LLC, Raritan, New Jersey: Employment, Equity Ownership. Lejeune:Janssen Scientific Affairs: Research Funding. Schein:Johnson & Johnson: Employment, Equity Ownership, Other: Own in excess of $10,000 of J&J stock. Wildgoose:Janssen Scientific Affairs, LLC, Raritan, New Jersey: Employment, Equity Ownership. Lefebvre:Janssen Scientific Affairs: Research Funding. Kaatz:Bristol Myer Squibb: Honoraria; Pfizer: Honoraria; CSL Behring: Honoraria; Boehringer Ingelheim: Consultancy; Pfizer: Consultancy; Janssen: Consultancy; Daiichi Sankyo: Consultancy; Bristol-Myers Squibb: Consultancy; Boehringer Ingelheim: Honoraria; Janssen: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal