Abstract

Introduction: Portal vein thrombosis (PVT) is a well-known complication caused by disturbed portal flows and hemostatic imbalances in liver cirrhosis (LC). Low molecular-weight heparin (LMWH) can be used as a treatment of PVT, but knowledge the about efficacy and safety of LMWH for LC patients remains limited. The aim of this study is therefore to investigate the clinical outcomes of cirrhotic patients with PVT treated with LMWH.
Method: From September of 2013 to December of 2015, LC patients who had PVT were treated with therapeutic doses of LMWH, dalteparin or enoxaparin for six months. Patients with severely decompensated LC, a history of major bleeding in the last six months, and/or impaired renal function were excluded.
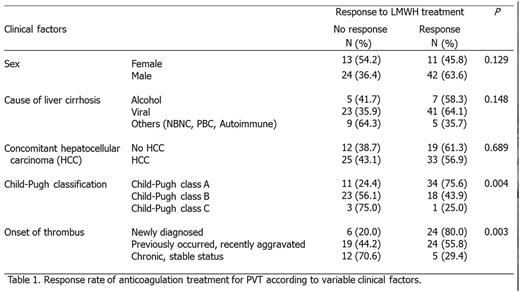
Results: Ninety patients were enrolled. The median age was 63.5 years (range 38-65), and male patients numbered 66 (73.3%). The most common cause of LC was hepatitis B virus infection (55 patients, 61.1%), followed by alcohol abuse (12 patients, 13.3%). Fifty-eight patients (64.4%) had hepatocellular carcinoma. Half of the patients had Child-Pugh class A cirrhosis, and 41 patients (45.6%) had class B cirrhosis. Thirty patients had thrombocytopenia with platelet counts less than 50,000/mm3. All patients had thrombus in the main trunk or in branches of the portal vein. Splenic vein involvement was confirmed in four patients, and 25 patients had superior mesenteric vein thrombus. PVT was newly discovered in 30 patients (33.3%), previously established but recently progressed was found in 43 (47.8%), and chronic but stable thrombus was noted in 17 (18.9%). The median time from the initial diagnosis of PVT to the start of anticoagulation therapy was 8.7 months (range: 0-125.9 months). Dalteparin was prescribed to 81 patients (90.0%) and enoxaparin to 9 (10.0%). The median duration of treatment was 5.8 months (range: 1-34.6 months). The overall rate of recanalization was 58.9%. Complete recanalization was reported in 16 patients (17.8%) and partial recanalization in 37 (41.1%). Patients with a favorable Child-Pugh class and recently diagnosed thrombus showed significantly better responses (Table 1). Concomitant hepatocellular carcinoma had no effect on the recanalization rate. In the patients who responded to anticoagulation therapy, the post-treatment laboratory findings including serum bilirubin and albumin were slightly improved compared to the pre-treatment state. At the time of the analysis, 48 patients (53.3%) had finished six months of the initial LMWH treatment as scheduled, while treatments for five patients were ongoing. The relapse rate of PVT was 56.6%, and the median time from the cessation of anticoagulation to relapse was 4.2 months (range: 1.4-7.0 months). Eight patients (8.9%) suspended their use of LMWH due to adverse events. The most common adverse event was bleeding, which was reported in 13 patients (14.4%). A history of variceal bleeding was a significant risk factor for hemorrhagic complications. Patients denoted as Child-Pugh Classes B or C showed a higher incidence rate compared to those designated as Class A. Two patients died due to fatal bleeding events, which were in these cases intractable duodenal variceal bleeding and intracranial hemorrhage.
Conclusion: Anticoagulation therapy using LMWH for PVT in LC is effective, with a recanalization rate of 59.6%. Advanced LC and a delayed start of anticoagulation since the initial diagnosis of PVT disrupted the recanalization effect of LMWH. Long-term maintenance of anticoagulation should be considered owing to the high recurrence rates, but much care is necessary with regard to hemorrhagic complications in patients with a past history of variceal bleeding.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal