Abstract
Background:While overt cerebrovascular accidents (CVAs) are well recognized in patients with Sickle Cell Anemia (SCA), more subtle cerebrovascular diseases, including neurocognitive performance deficits and silent cerebral infarcts (SCIs), are present but less well understood, particularly in adults. SCI manifests as asymptomatic white matter hyperintensities (WMH) found on T2-weighted, diffusion-weighted or Fluid Attenuated Inversion Recovery (FLAIR) magnetic resonance images. WMH volume has been found to be negatively associated with IQ in SCA. We sought to clarify the role of WMH load by MRI using region of interest volume calculations in patients particularly at risk, adult patients with SCA.
Methods: SCA (HbSS/HbSβ0) and AA subjects, ages 18-55 years old, with no evidence of TIA/Stroke, prothrombotic history, clotting or bleeding disorder, and not on anticoagulation were recruited. Hydroxyurea use was noted but was neither an inclusion nor exclusion criterion. Evaluation included a routine questionnaire for basic social, educational and health information. Steady state laboratory evaluation was obtained within one week of imaging. Neurocognitive performance was evaluated by the Cogstate battery at the time of the MRI. Cogstate analysis included tests of executive function (the Groton Maze Learning Test or GMLT), recall, social and emotional cognition and learning. 3T MRI included 3D-T1w , T2, FLAIR, pseudo-continuous arterial spin labeling and diffusion tensor imaging (DTI). Fractional anisotropy (FA) and mean diffusivity (MD) were extracted from DTI data and calculated for gray matter (GM) and white matter (WM). Cerebral blood flow (CBF) was also calculated for GM and WM separately. FLAIR images were reviewed (reviewer was blind for group) for WMHs using the NIH image analysis package MIPAV (http://mipav.cit.nih.gov/). WMH signal regions (ROI) were identified and selected/masked using the 'levelSet' ROI function on a slice-by-slice basis. ROIs were grouped, and average WMH volume (using slice thickness) calculated for each subject using the MIPAV Statistics Generator.
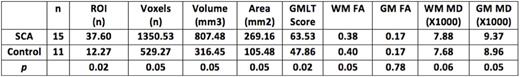
Results:15 SCA and 11 AA subjects were recruited for the tailored questionnaire, 3T MRI, routine laboratory testing and neurocognitive testing. Both number and volume of ROI were increased in SCA patients (p=0.018 and p=0.052 respectively). GM and WM CBF were markedly increased in SCA patients (p=0.005 for both). GM-MD was increased in SCA patients (p=0.046) while increases in WM-FA and MD were of borderline significance (p=0.055 and p=0.564) respectively. These data are shown in the Table below. Although SCA patients fared significantly worse on the GMLT, p=0.020, there was no association of the GMLT with ROI volume (p=0.96). ROI volume was positively associated with MCHC (p=0.035), a dense cell biomarker, but we could not find an association with Hb, indirect bilirubin or reticulocyte count. MDWM FA and GM-MD also correlated significantly with MCHC but the major associations of DTI measurements, like those of both grey matter (GM) and white matter (WM) cerebral blood flow, were correlated with Hb levels (both GM and WM MD, p=0.004). There was no association of oxygen saturation or change in oxygen saturation with ROI number of volume.
Conclusions: The etiology of the documented cognitive difference between SCA and HbA is unclear. Although there is some suggestion that WMH correlates with SCA outcome and may explain this discrepancy, the association is weak. We could not find as association of ROI number or ROI volume with cognitive outcome, nor could we find an association of ROI volume with any pertinent laboratory parameters except MCHC. Unlike CBF, WMH volume load, as represented by ROI volume, does not appear to correlate with the degree of anemia or with clinical disease. Whether cognitive impairment requires a "second hit" or whether it is multifactorial in nature, stemming from chronic oxidative stress, intermittent hypoxia or other factors, remains to be determined.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal