Abstract
Background: Contraception and pregnancy planning are critically important for patients with sickle cell disease (SCD). However, rates of contraceptive utilization are often suboptimal and unplanned pregnancy remains a problem among this patient population. In an effort to improve care, a multidisciplinary hematology and gynecology clinic was initiated at University Hospitals Case Medical Center in which women of reproductive age received comprehensive care in single visits.
Objective: To determine the impact on pregnancy, contraception use and sexually transmitted infections (STIs) diagnoses of a multidisciplinary hematology and gynecology clinic for women with SCD.
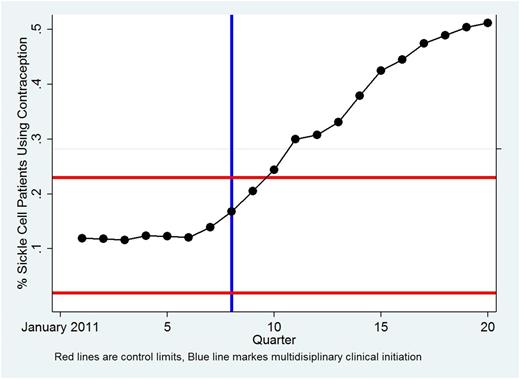
Methods: A retrospective cohort study of women seen in University Hospitals Hematology Clinic for sickle cell disease from 2011 to 2015. Baseline demographics as well as the subsequent outcomes of pregnancies, contraception use and STIs were collected. Total differences in outcomes before and after the multidisciplinary clinical were evaluated with Fisher's exact test. Longitudinal differences in pregnancies and STIs were analyzed with time-to-event analyses. For outcomes of interest p charts were constructed with upper and lower control limits.
Results: A total of 133 women total were identified as reproductive age women with sickle cell disease from 2011 to 2015. The percentage of SCD patients using birth control before and after the multidisciplinary clinic increased from 12.3% to 37% (p=0.0001). The p chart for contraception use is provided bellow and was highly significant. No significant differences in pregnancy or STIs were identified in time-to-event analysis and p charts, though the total number of STIs before and after the intervention was limited (eighteen).
Conclusion: Incorporating a multidisciplinary approach with combined hematology and gynecology care for women with sickle cell disease has the potential to improve access to contraception use in this population.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal