Abstract
Introduction: Sickle cell disease (SCD), an inherited blood disorder, is characterized by episodes of painful vaso-occlusive crises (VOC). Peripheral vasoconstriction may contribute to VOC by prolonging the transit time of red blood cells through the microvasculature. We recently demonstrated that heat-induced pain produces stronger vasoconstriction in SCD subjects versus controls, suggesting abnormal autonomic regulation of regional blood flow in SCD. Thus, although pain is generally thought to be a consequence of VOC, it is possible that pain itself may trigger a cascade of events that leads to large-scale VOC by promoting regional peripheral vasoconstriction.
Objective: To determine if the underlying functional mechanisms of the vasoconstriction response to heat-induced pain in SCD differ from normal controls.
Experimental Protocols: 22 SCD and 23 control (healthy and sickle cell trait) subjects were recruited at Children's Hospital of Los Angeles. Quasi-periodic pulses of pain were delivered on the right forearm using TSA-II neuro analyzer heating thermode. Electrocardiogram, respiration, continuous blood pressure and photoplethysmogram (PPG) were recorded. Both blood pressure and PPG were measured on the ring finger and thumb on the contralateral hand. Reductions in PPG amplitude were taken to represent vasoconstriction.
Analysis: A mathematical model was applied to the data to extract the key parameters relating the thermal (pain) pulses, blood pressure and respiration to vasoconstriction. The model enabled the vasoconstriction response to pain to be decomposed into: 1) a neurogenic component, measuring the direct effect of the thermal pain pulse on vasoconstriction; 2) a local vascular component, relating fluctuations in blood pressure, induced by pain, to vasoconstriction; 3) a neurogenic-vascular interaction component, reflecting the modulation of the vascular component by the pain stimulus; and 4) a respiratory coupling component.
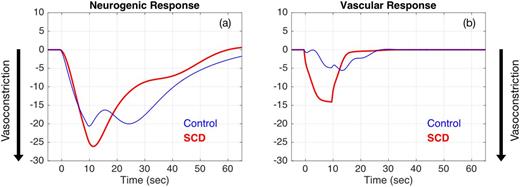
Results: The model predicted stronger vasoconstriction responses to heat pain in SCD than controls (p = 0.002), consistent with the previous results reported by Khaleel et al. (Blood 126 (23):67, 2015). The pattern of the neurogenic response in both groups was similar but stronger in SCD (Fig 1a). The time-course of the local vascular component was quite pronounced in SCD (Fig 1b) - increases in blood pressure promoted stronger and more rapid vasoconstriction in SCD relative to controls. The neurogenic-vascular interaction (not shown) caused further peripheral vasoconstriction in SCD, but tended to reduce vasoconstriction in controls. The respiratory contribution was small in both groups.
Discussion & Conclusions: Heat-induced pain produces peripheral vasoconstriction via direct autonomic nervous system activation, as well as indirectly through the local vascular response to pain-triggered blood pressure fluctuations. The complex dynamics of the vasoconstriction response can only be understood by application of a mathematical model incorporating several relevant simultaneously measured and frequently sampled physiological signals. The stronger neurogenic response in SCD suggests elevated sympathetic activity compared to controls. The local vascular component in the SCD subjects exhibits a higher reactivity to increases in local blood pressure that promotes vasoconstriction, consistent with underlying endothelial dysfunction. The contribution of neurogenic-vascular interaction derived from the model likely represents the degree to which sympathetic overactivity leads to vascular dysfunction in SCD. These results suggest that dysautonomia and its interaction with peripheral vascular dysregulation participate in the genesis of vaso-occlusive crisis.
(a) average neurogenic response (% change from baseline) to a heat pain pulse (20 °C, 10-sec long) in SCD (N = 22) and controls (N = 23); (b) average vascular response (% change from baseline) to a blood pressure pulse induced by pain (10 mmHg, 10-sec long) in SCD and controls.
(a) average neurogenic response (% change from baseline) to a heat pain pulse (20 °C, 10-sec long) in SCD (N = 22) and controls (N = 23); (b) average vascular response (% change from baseline) to a blood pressure pulse induced by pain (10 mmHg, 10-sec long) in SCD and controls.
Wood:Biomed Informatics: Consultancy; AMAG: Consultancy; Vifor: Consultancy; Ionis Pharmaceuticals: Consultancy; Vifor: Consultancy; World Care Clinical: Consultancy; Celgene: Consultancy; Biomed Informatics: Consultancy; AMAG: Consultancy; Apopharma: Consultancy; Apopharma: Consultancy; World Care Clinical: Consultancy; Celgene: Consultancy; Ionis Pharmaceuticals: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal