Abstract
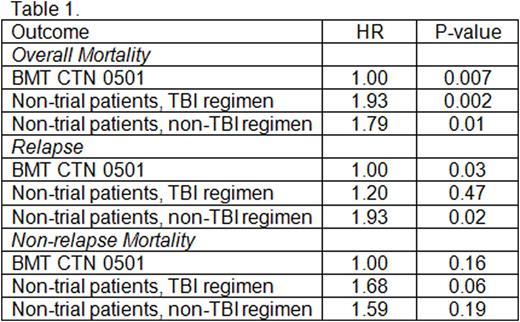
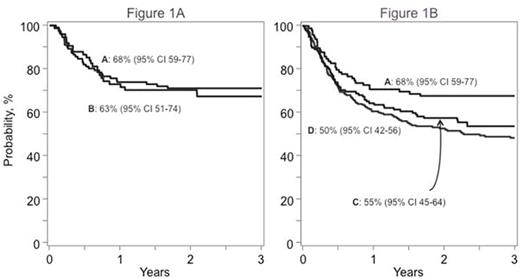
The Blood and Marrow Transplant Clinical Trials Network (BMT CTN 0501; NCT00412360) randomized children with hematologic malignancy to one or two cord blood unit transplantation between December 2006 and February 2012. While the trial concluded that survival was similar regardless of number of units infused, results were generally better than those previously reported after single UCB transplant. The apparently improved survival in recipients of BMT CTN 0501 compared to prior studies in children transplanted with a single UCB unit prompted a comparison of trial versus non-trial treatment outcomes to determine 1) the generalizability of trial results and 2) whether survival was better for patients treated with the trial regimen. Using data reported to the Center for International Blood and Marrow Transplant Research during the trial period, 396 recipients of one UCB unit transplant met the broad eligibility criteria for BMT CTN 0501 (i.e. aged 1- 21 years, high-risk acute leukemia, performance score ≥70). Trial and non-trial patients were comparable in their HCT-CI score. Trial patients (n=100) received total body irradiation (TBI) 1320 cGy, cyclophosphamide 120 mg/kg, and fludarabine 75 mg/m2 (TCF). Non-trial patients either received the same regimen as in the trial (N=62; non-trial TCF) or an alternative regimen (N=334; non-trial non-TCF regimen). Excluded were 13 patients on BMT CTN 0501 randomized to receive a single UCB unit for malignant diseases other than acute leukemia. Patient and disease characteristics of those treated on BMT CTN 0501 and others were similar except that those who received non-trial TCF regimen were more likely to report performance scores of 80 or 70 (24% versus 11%, p=0.04) and transplanted in relapse (18% vs. 5%, p=0.02) and those that received non-TCF regimens were more likely to 1-10 years of age (76% versus 53%, p<0.0001). Sixty-three percent of non-trial non-TCF regimens included TBI (≥1000 cGy) and the predominant non-TBI regimen was busulfan and cyclophosphamide. All patients received a calcineurin inhibitor for graft-versus-host disease (GVHD) prophylaxis. Donor-recipient HLA-match, median infused total nucleated cells and median follow up times were similar across the groups. Three-year survival rates were similar between patients receiving TCF regimen either on (A) or off trial (B), Figure1A, p=0.83. Similarly, there were no differences in hematopoietic recovery, relapse or non-relapse mortality between trial and non-trial TCF. However, compared to TCF on trial (A), overall survival rates were significantly lower with non-TCF non-TBI (C) and TBI (D) containing regimens after adjusting for age, CMV serostatus, disease and disease status; Figure 1B, 68% versus 55% (p=0.001) and 68% versus 50% (p=0.04), respectively. Results of multivariate analysis are shown in Table 1. Compared to patients treated on trial (TCF regimen; 20% at 3-years) relapse rates were higher with non-TCF non-TBI (42%, p=0.003) but not TBI-containing regimens (25%, p=0.38) after adjusting for age, disease, disease status and CMV seropositivity. Among non-TCF patients, relapse risk was higher for non-TBI compared to TBI-containing regimens (hazard ratio [HR] 1.61, p=0.02) but not mortality risk (HR 0.93, p=0.74). Cytogenetic risk features were not associated with relapse or survival. There were no differences in hematopoietic recovery, acute and chronic GVHD. The results of BMT CTN 0501 appear generalizable to the population of trial eligible patients. The survival differences between the trial specified and other conditioning regimens support use of the TCF regimen to improve survival. It also indicates the importance of conditioning regimen for outcome and may serve as a stimulus to design trials to identify the optimal regimen for children with acute leukemia undergoing UCB transplantation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal