Abstract
Introduction:Diffuse large B-cell lymphoma (DLBCL) is the largest subgroup of malignant lymphoma. Prognosis has increased after introduction of rituximab, and today more than 80% of the patients will achieve partial or complete remission after standard immunochemotherapy. However, approximately 30% will either present with refractory disease or develop relapse. The standard approach for younger patients with relapsed disease and without major comorbidity is salvage treatment followed by high dose therapy with autologous stem cell transplant (ASCT). This potentially curative treatment is toxic with many side effects, and social outcomes for patients need to be investigated.
Objectives:Patients with relapse of de novo DLBCL and transformed indolent lymphoma (TIL) were included. The aim was to describe social outcome after ASCT in form of return to work (RTW).
Methods: Patients with B-cell lymphoma in the period 2000-2012, who received ASCT as relapse treatment, were extracted from the Danish National Lymphoma Registry. Medical records were reviewed for clinical, pathological, and treatment information. Individual information on socioeconomic factors and social outcomes were achieved by cross-reference to national administrative registries. Patients were included in RTW analyses, if they received public welfare benefits in at least four weeks including the week of stem cell reinfusion. RTW was defined as four consecutive weeks without receiving welfare benefits; retirement, disability pension and death was regarded as competing events. Patients were followed until RTW, emigration, permanent withdrawal from the labour market, death, or December 31, 2015, whichever came first.
Results: A total of 369 patients were identified. At the time of ASCT, 164 (44%) patients received public welfare benefits in form of either sick leave or unemployment benefits. Furthermore, 61 (17%) received disability pension or similar, 102 (28%) received old age pension, and 41(11%) patients did not receive any welfare benefits.
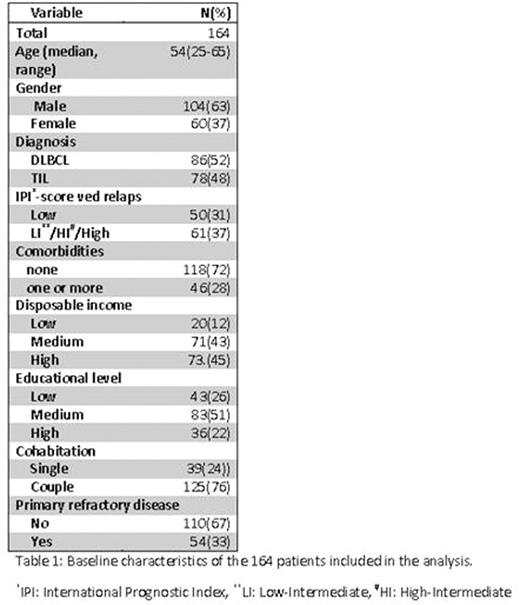
The 164 patients receiving sick leave or unemployment benefits were included in the analysis. Median age was 54 years (25-65), 16 patients were above the age of 60, and 104 were male (64%). A total of 54 patients had primary refractory disease; median time to relapse was 1.7 years. Both diagnoses were equally represented with 78 (48%) patients with TIL, IPI score at relapse was available for 118 patients, 22 % had a score of high-intermediate or high. Furthermore, socioeconomic factors at time of relapse showed, that 36 (22%) patients had only basic (mandatory) education, 39 (24%) patients lived alone and 60 (37%) patients had a low disposable income, corresponding to the 1st or 2nd quintile of the Danish population with the same gender and in the same age-group. Most of the patients, n=118 (72%), did not have comorbidities, but 46 patients had one or more at time of relapse. (Table 1)
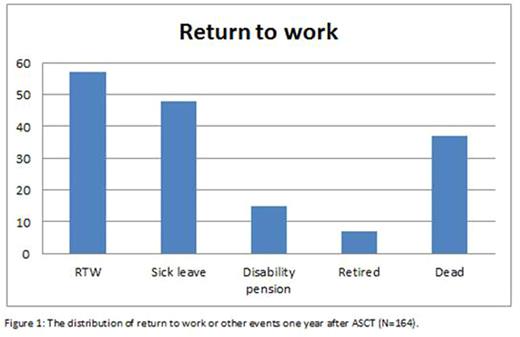
Median time to return to work was 420 days, ranging from 13 to 909 days. One year after year after ASCT, 57 (35%) patients had returned to work, 15 (10%) received disability pension, and 7 (4%) received old age pension. A total of 48 (29%) were still on sick leave, and 37 (23%) had died. (Figure 1)
Conclusion: In this nationwide population based study we found that after one year only 35% of the patients had returned to work, 14% had been retired and 23% had died. This emphasizes that this patient group is at risk of impaired social status. There is an unmet need of focused social rehabilitation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal