Abstract

Introduction
GVHD-free, relapse-free survival (GRFS) has been previously developed as a novel composite endpoint designed as a measure of transplant effectiveness, which attempts to take into account the morbidity associated with GVHD (Holtan et al. Blood 2015). The conventional definition of GRFS however considers grade 3-4 acute GVHD and immunosuppression-requiring chronic GVHD (cGVHD) as static endpoints, whereas in reality these outcomes are often reversible. Patients with short-lived GVHD are considered treatment failures, which may not represent an accurate measure of transplant success. Therefore, we have developed a statistical method that provides an estimate of the probability, at any time post-transplant, of being alive, in remission, and without clinically significant cGVHD, defined as moderate-severe by the NIH consensus criteria.
Methods
In this new composite endpoint, which we call current GRFS (CGRFS), death and relapse are treated as terminal events, while cGVHD is considered a dynamic event, which can "resolve" once manifestations are quiescent and systemic immunosuppression discontinued. Grade 3-4 acute GVHD was intentionally not included in this endpoint, as this event almost universally will either resolve with time or convert to either death or cGVHD, which are both captured as part of CGRFS. Statistically, the CGRFS was defined as the sum of the survival without evidence of relapse and moderate-severe cGVHD and the probability that one recovered from moderate-severe cGVHD. The probability that one recovered from moderate-severe cGVHD was calculated by looking at the differences of relevant Kaplan-Meier estimates. Comparison of CGRFS between two independent samples was implemented by the simulation-based supremum test.
Results
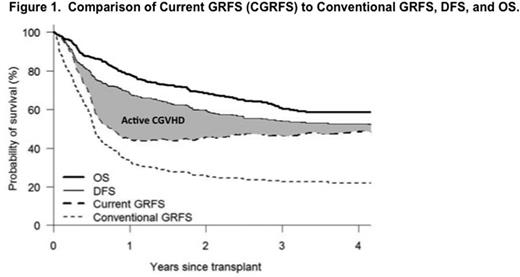
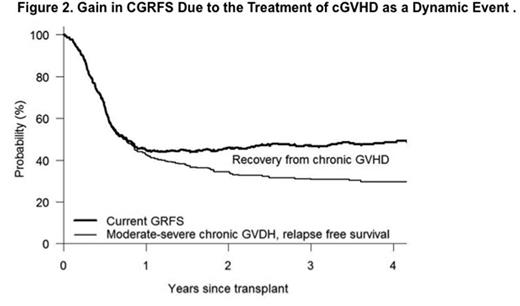
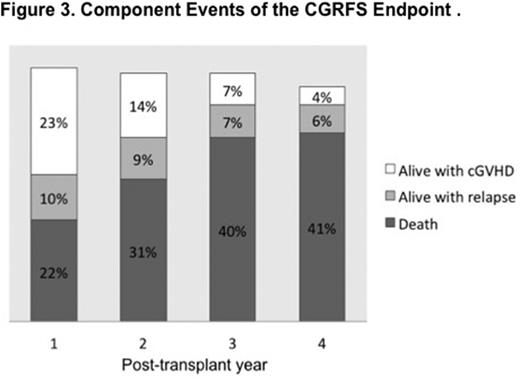
We evaluated 437 consecutive patients receiving an allogeneic hematopoietic stem cell transplant at a single institution from a matched related (MRD, n=125), matched unrelated (MUD, n=165), or haploidentical (HID, n=132) donor between January 2010 and July 2015. Transplant recipients had a median age of 54 years (range 18-77), DRI high/very high in 30%, and HCT-CI ³3 in 46%. Myeloablative conditioning was used in 50% and PBSC was the stem cell source in 78%. GVHD was prospectively documented by a dedicated practitioner on an ongoing basis. With a median follow-up time of 36 months, estimated 3-yr overall and disease-free survival was 61% and 54%, respectively. Conventionally defined GRFS at 1, 2, 3 and 4 years was 33%, 26%, 23%, and 22% respectively. In contrast, when moderate-severe cGVHD was treated as a dynamic event, corresponding CGRFS was 45%, 46%, 47% and 49%, respectively (Figure 1). The corresponding gain in CGRFS survival, due to the treatment of cGVHD as a dynamic event, was 12%, 20%, 24% and 27% respectively (Figure 2). Patients living with active mod-severe cGVHD decreased over time, quantitated at 23%, 14%, 7% and 4% respectively at 1, 2, 3 and 4 years post-transplant (Figure 3). CGRFS was significantly correlated with DRI (low/intermediate vs. high/very high, p<0.01), but not transplant type, age, HCT-CI, graft source, regimen intensity or year of transplant.
Conclusion
Whereas only a third of patients achieve "transplant success" by conventional 1-yr GRFS, nearly half of patients by CGRFS are considered cured without the morbidity of ongoing GVHD. We propose that CGRFS may represent are more accurate estimate of transplant effectiveness.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal