Abstract
Background: Diffuse large B cell lymphoma (DLBCL) is the most common type of non Hodgkin lymphoma (NHL).Nearly 50% of high-risk DLBCL patients are not cured with standard rituximab, cyclophosphamide, doxorubicin, vincristine and prednisone (RCHOP). High risk DLBCL may be defined as double hit lymphoma (DHL, translocation of MYC and BCL2 or BCL6), double expressor lymphoma (DEL, over expression of MYC and BCL2), high risk international prognostic index (IPI) of 3-5, high Ki-67, and non-germinal center subtype (non-GCB). The majority of DHL cases occur in the GCB subtype, as opposed to the majority of DEL cases which occur in non-GCB. Hence we sought to compare different high risk subsets treated with dose-adjusted etoposide, doxorubicin, cyclophosphamide, vincristine, prednisone and rituximab (DA) EPOCH-R. In single arm phase II clinical trials, dose adjusted (DA) EPOCH-R has shown promising results, with potential greater efficacy in the GCB subtype in subset analyses (Wilson et al, Hematologica 2012). A randomized phase III study comparing RCHOP with (DA) EPOCH-R in newly diagnosed DLBCL has completed accrual, with highly anticipated results due in late 2016.
Methods: We conducted a retrospective reviewof all consecutive, newly diagnosed DLBCL patients treated with (DA) EPOCH-R at MD Anderson Cancer Center from 2010 to 2014. Eligible patients were 18 years or greater, had high-risk DLBCL as determined by the treating physician, and had available data of treatment and response. The cell of origin subtype was determined by immunohistochemistry using Hans algorithm, and MYC and BCL2 positivity were defined as BCL2 positive in at least 70% and MYC positive in at least 40% of cells. DHL was defined as rearrangement of MYC and BCL2 or BCL6 by fluorescent in situ hybridization. The objectives were to analyze demographic, prognostic, and treatment variables in comparison with clinical response and survival outcomes in three sub groups which included 1. DHL (GCB) 2. DLBCL without MYC and BCL2 expression (GCB), and 3. DEL (GCB and non GCB). Complete response (CR), overall survival (OS) and progression free survival (PFS) were calculated using standard methods. Statistical analysis was done using Fishers exact test or Chi-square test / Kruskal-Wallis test. Kaplan-Meier method was used for time-to-event analysis including overall survival and progression free survival. The Log-rank test was used to evaluate the difference in time-to-event endpoints between patient groups.
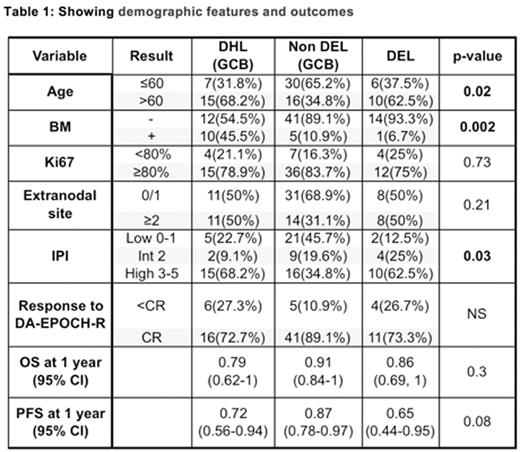
Results: We identified 233 high risk DLBCL patients treated with (DA) EPOCH-R. After filtering the data to identify patients which were included in our three groups, we identified 22 patients with DHL (GCB), 46 patients with non DEL (GCB), and 16 with DEL. The demographic features and outcomes are mentioned in the table 1 below. The DHL group had more frequent bone marrow (BM) involvement, and the DHL and DEL groups were more frequently age >60 years and high IPI in comparison to the non DEL GCB group. The CR rate, OS and PFS at 1 year were not significantly different between these three groups. Figure 1 highlights the OS (A) and PFS (B) results of each group.
Conclusions: (DA) EPOCH-R is highly effective in patients with subsets of patients with high-risk DLBCL and may be able to overcome prognostic factors which have been shown to be adverse with RCHOP therapy. The results of this retrospective study suggest that OS in DHL, DEL and non DEL (GCB) are not statistically different. Hence, intensive chemotherapy with (DA) EPOCH-R could be considered as a frontline treatment option for patients with high risk DLBCL, pending further confirmation in randomized trials.
Oki:Novartis: Research Funding. Fowler:Infinity: Consultancy, Research Funding; Roche: Consultancy, Research Funding; TG Therapeutics: Consultancy; Celgene: Consultancy, Research Funding; Jannsen: Consultancy, Research Funding; Gilead: Research Funding. Wang:Pharmacyclics: Research Funding; Juno Therapeutics: Research Funding; Acerta Pharma: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Celgene: Research Funding; BeiGene: Research Funding; Kite Pharma: Research Funding; Onyx: Research Funding; Asana BioSciences: Research Funding; Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding. Fayad:Seattle Genetics: Consultancy, Research Funding. Westin:ProNAi: Membership on an entity's Board of Directors or advisory committees; Spectrum: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Chugai: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal