Abstract
Individuals with SCD have recurrent episodes of ischemia-reperfusion in vital organs, and abnormal microcirculation is considered a major determinant of end organ damage. Hydroxyurea (HU) treatment has been shown to produce ATP- and nitric oxide-mediated vasodilation, and to improve red cells deformability Few tools are available to quantitatively measure microvascular blood flow in vivo. The purpose of this study was to assess the ability of a novel ECHO based imaging modality to assess the effect of hydroxyurea on cardiac and skeletal muscle perfusion in patients with sickle cell anemia.
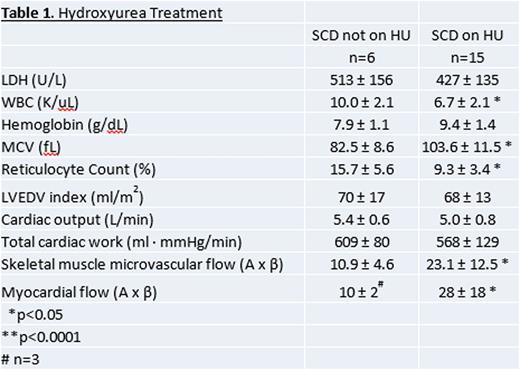
Methods and Results: Twenty-one HBSS/B0 patients, of whom 15 were treated with HU(average daily dose of 18 ± 8 mg/kg/day), underwent brachial artery ultrasound, echocardiography and contrast enhanced ultrasound (CEU) perfusion imaging of deep flexor muscles of the forearm as well as the myocardium at rest and during vasodilator stress with regadenoson ( ClinicalTrials.gov NCT016028090). Quantitative image analysis was performed to obtain microvascular blood volume and flow velocity measurements. Patients on HU had a lower white blood cell count (6.7±2.1 K/uL vs 10.0±2.1 K/uL, p<0.05), higher mean corpuscular volume (103.6±11.5 fL vs 82.5±8.6 fL, p<0.05) , and lower reticulocyte count (9.3±3.4% vs 15.7±5.6%, p<0.05) as well as a trend towards higher hemoglobin (9.4±1.4g/dL vs 7.9±1.1g/dL , p=NS). Table 1. Cardiac output and total myocardial work was not affected by HU treatment and macrovascular flow in the brachial artery was not affected (Figure 1A). In contrast, both skeletal muscle microvascular flow and myocardial microvascular flow was significantly higher in the SCD patients on HU therapy (Figure 1B, 1C).
Conclusions: The beneficial effects of HU therapy in SCD are varied, and clinical effects are often seen prior to a rise in fetal hemoglobin. Other effects, such as lower hemolysis, improved red cell deformability, and inhibition of adhesive properties in the microvasculature have been reported. Some of the beneficial effects of HU may be due to stimulation of nitric oxide synthase, induction of cyclic GMP dependent signaling and improved NO bioavailability. Our study indicates that SCD patients on chronic HU therapy have higher levels of myocardial and skeletal muscle microvascular blood flow. Long term studies are necessary to evaluate whether HU reduces end organ damage in SCA.
Skeletal muscle and myocardial microvascular blood flow.
Each panel shows blood flow in all SCD patients (red filled diamonds), SCD patients not on HU (red open triangles) and SCD patients on HU (red open inverted triangles).
Panel A. Skeletal muscle perfusion normalized to hemoglobin (A x β x hemoglobin)
Panel B. Myocardial perfusion normalized to hemoglobin level and total myocardial work.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal