Abstract
Despite being a monogenic disease, sickle cell anemia (SCA) is remarkably heterogeneous in its phenotypic expression. Additional genetic polymorphisms such as α-thalassemia co-inheritance and β-globin haplotypes have a recognized influence. Alpha-thalassemia reduces HbS polymerization and decreases hemolysis by lowering intracellular hemoglobin concentration. The three major β-globin haplotypes, Senegal (SEN), Benin (BEN) and Bantu/Central African Republic (CAR), have been reported to affect disease severity, in part by influencing baseline HbF levels, but no studies in large cohorts have so far compared the biological parameters in patients with these haplotypes. The haplotype BEN is largely predominant in the US, and patients are often compound heterozygotes for two different haplotypes, whereas the haplotype CAR is rarely observed. In Africa, environmental, nutritional and infectious factors make it difficult to distinguish the role of haplotypes in modulating hematological characteristics. In France, SCA-patients are frequently homozygous for the different haplotypes, rendering the comparison of hematological parameters possible. The aim of this study was to evaluate the impact of α-thalassemia and β-haplotypes on the biological parameters recorded at baseline and on hydroxyurea (HU).
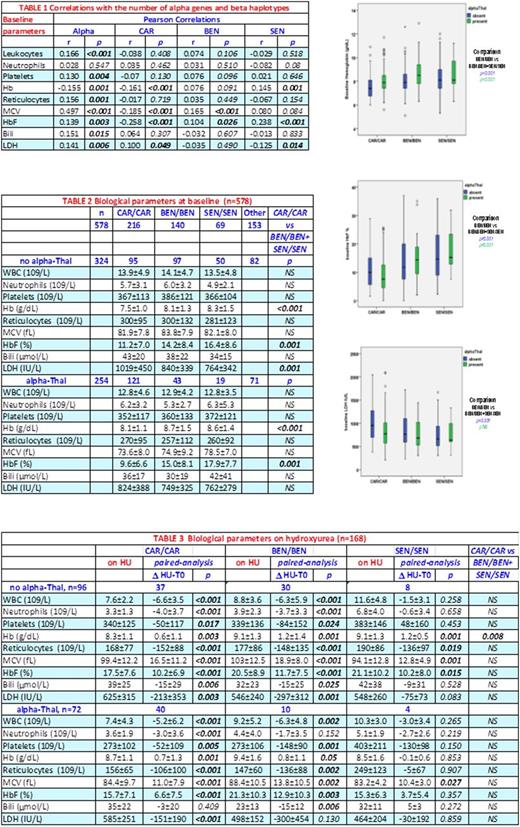
SCA-patients from the Créteil pediatric cohort with available assessment of α genes, β-haplotypes and baseline parameters were included in this study (n=578). Alpha-thalassemia was present in 254/578 (44%), with 191 (33%) having one deleted gene and 63 (10.9%) two. CAR/CAR homozygosity was present in 216 (37.4%), BEN/BEN in 140 (24.2%) and SEN/SEN in 69 (11.9%) patients, and 153 (26.5%) had other haplotypes (Cameroon, atypical or heterozygous). The presence of α-Thal was significantly more frequent (p<0.001) in CAR/CAR (121/216; 56%) than in BEN/BEN (43/140; 31%) and SEN/SEN (19/69, 28%). Univariate correlations of biological parameters with the number of α genes and β-haplotypes are shown in Table 1. Multivariate linear regression analysis showed that HbF% was positively correlated with SEN (β=0.152,p=0.003) and negatively with CAR (β=-0.189,p<0.001) whereas hemoglobin and LDH were inversely correlated with the number of α genes (β=-0.225,p<0.001 and β=0.201,p<0.001) and CAR haplotypes (β=-0.230,p<0.001 and β=0.171,p=0.001) respectively. As shown in Table 2, hemoglobin and HbF% were significantly lower in CAR/CAR than in BEN/BEN, and lower in BEN/BEN than in SEN/SEN, independently of the α-Thal status. Whereas LDH was not different in patients with α-Thal, LDH was significantly higher in CAR/CAR than in BEN/BEN and SEN/SEN in those with no α-Thal. Thus, the CAR/CAR patients with no α-Thal have the most severe hemolytic anemia with the lowest Hb and highest LDH levels.
Hydroxyurea was given to 168 SCA-children at the median age of 6.6 years and the median dose of 26 mg/kg/day for at least one year between February 1993 and December 2014. The biological parameters were recorded when HbF % increase was maximal, and the delta (D) values from the initiation levels were calculated. Indications for HU were frequent VOC/ACS (n=101), severe anemia (n=23), and normalized TCD in patients with abnormal-TCD history (n=44). Alpha-Thal was present in 72/168 (56%), while CAR/CAR was present in 77/168 (46%), BEN/BEN in 41/168 (24%), and SEN/SEN in 12/168 (7%). Table 3 summarizes the biological parameters and D changes. Paired analysis showed significant changes in all parameters whatever the β-haplotypes and α gene number. Leukocytes, neutrophils, platelets, reticulocytes, bilirubin, LDH were lower while hemoglobin, MCV and HbF were higher. However, the SEN/SEN/α-Thal group was too small to show significance. On HU, parameters were no longuer significantly different between CAR/CAR patients and the others, except for hemoglobin that remained significantly lower (p=0.008) in CAR/CAR patients without α-Thal than in BEN/BEN and SEN/SEN patients.
In conclusion, patients without α-Thal and with the CAR/CAR β-haplotype have the most severe hemolytic anemia at baseline. Despite a significant increase of their hemoglobin level on HU, they remain the most severely anemic patients. These results may explain some of the discrepancies observed between US and French studies, in particular regarding the effects of HU on cerebral vasculopathy for which the correction of anemia is crucial.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal